Introduction
Actinic keratosis (AK) is a precancerous skin lesion that develops due to chronic sun exposure. They are common in fair-skinned individuals and often appear on sun-exposed areas such as the face, alopecic scalp, ears, neck, and arms. Although most AKs remain stable, a small percentage can progress to cutaneous squamous cell carcinoma (SCC). Early detection and treatment are essential to prevent malignant transformation.
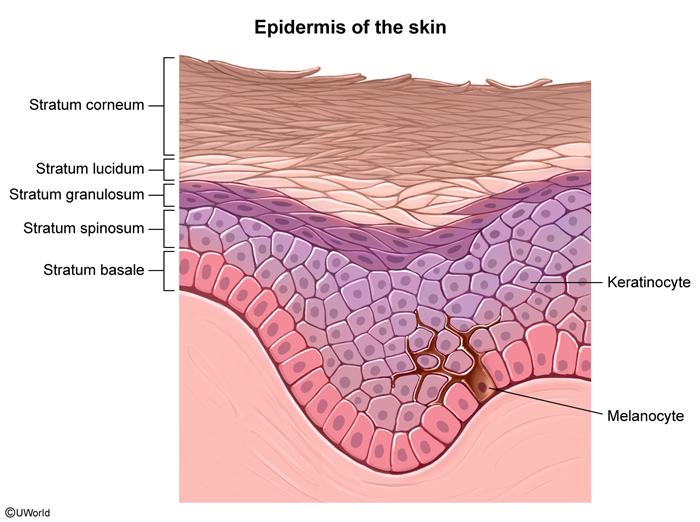
Pathophysiology
Chronic ultraviolet (UV) radiation exposure induces DNA damage in keratinocytes
Risk factors
- Chronic sun exposure/history of sunburns.
- Fair skin.
- Disorders of DNA repair (eg, xeroderma pigmentosum).
- Immunosuppression (eg, chronic immunosuppressive therapy).
- Advanced age.
Pathology
On histologic examination
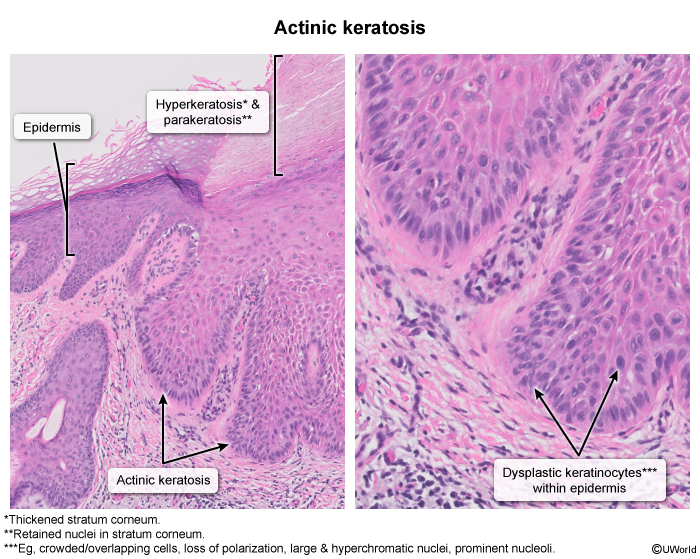
AKs are considered premalignant lesions on a continuum with SCC. The extent of epidermal involvement differentiates AK from SCC.
- AK: Atypical keratinocytes do not involve the full thickness of the epidermis.
- SCC in situ: Atypical keratinocytes involve the full thickness of the epidermis without infiltration into the dermis.
- Invasive SCC: Atypical keratinocytes involve the full thickness of the epidermis and penetrate through the epidermal basement membrane into the dermis or deeper tissues.
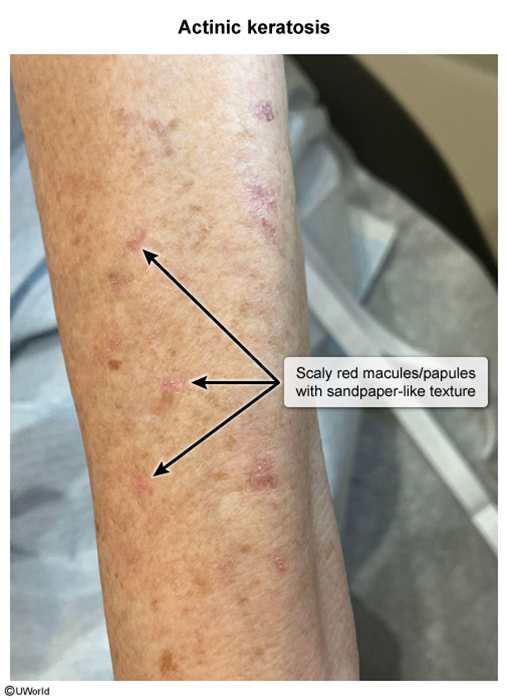
Clinical presentation
AKs most commonly present as erythematous papules with overlying white scales
Other less common subtypes of AK also exist.
- Hypertrophic: Erythematous plaque covered with thick scales (
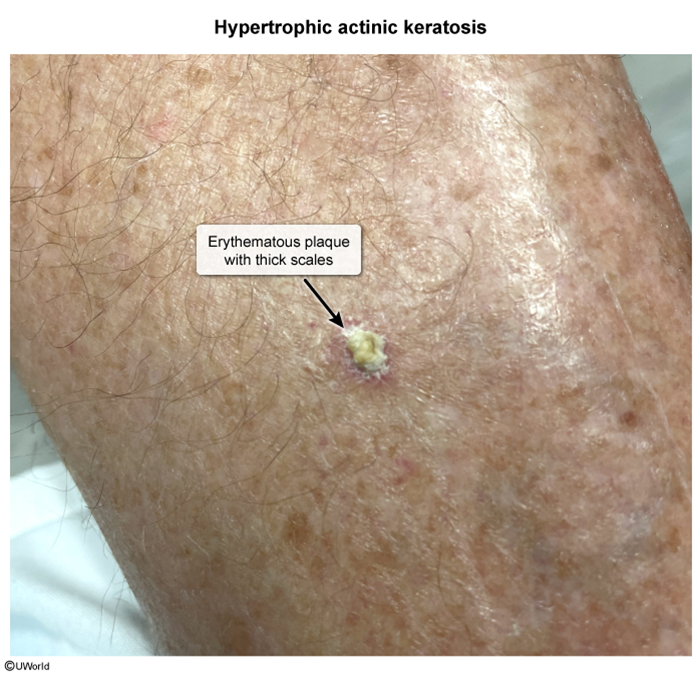 image 4
image 4 - Atrophic: Soft, red macule without scales.
- Cutaneous horn: Cone of keratin (straight or curved), typically with AK or SCC at its base (
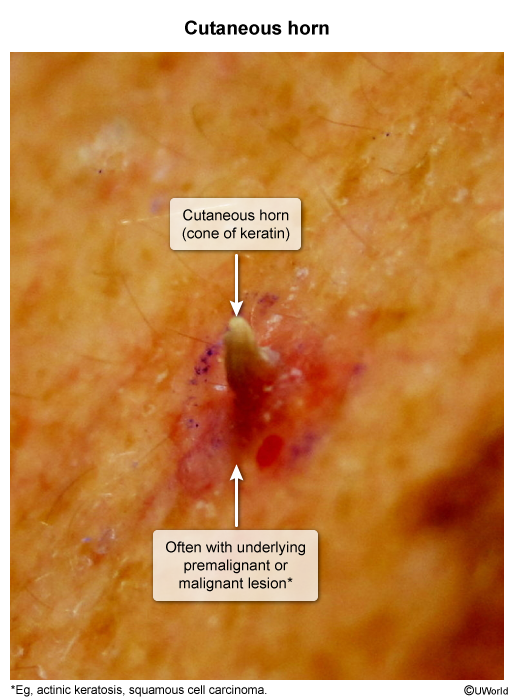 image 5
image 5 - Pigmented: Hyperpigmented macule or patch covered with scales (
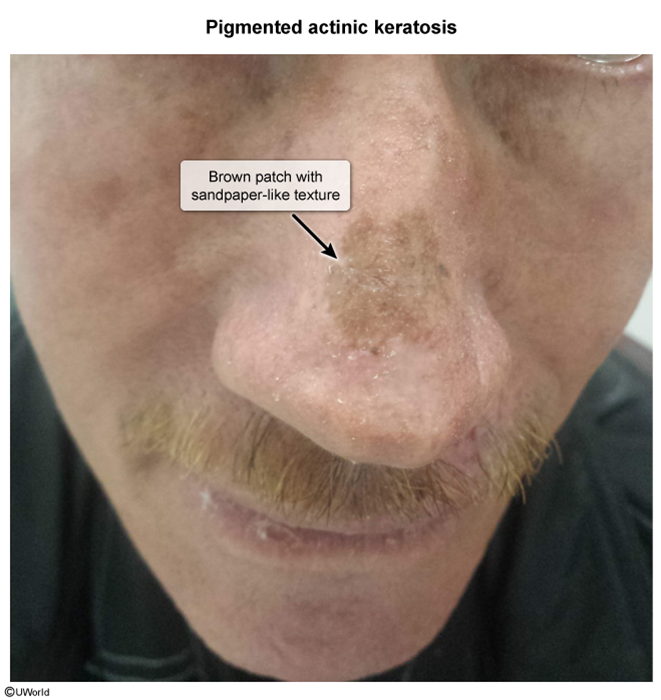 image 6
image 6 - Actinic cheilitis: Focal or diffuse scaly areas on the lips, with or without fissuring or ulceration (
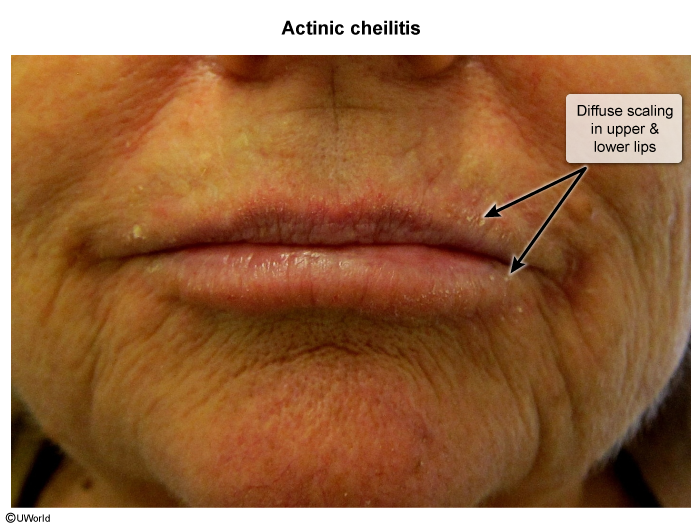 image 7
image 7
Diagnosis
A diagnosis is usually made based on the lesion's appearance; however, biopsy is indicated in select cases when differentiating AK from SCC is needed. In general, the following lesions should be biopsied to rule out SCC.
- Lesions ≥1 cm.
- Tenderness, induration, ulceration, or rapid growth of the lesion.
- Lesions that do not respond to treatment (see Management).
In addition, pigmented AKs may need biopsy to differentiate them from melanoma.
Differential diagnosis
- Seborrheic keratosis (SK): Often confused with AK because of the similarities of their names. SK typically presents as a brown "stuck-on" papule with a wart-like surface ( , not characteristic of AK. Although SK commonly presents in older individuals, it is not related to sun exposure and has no malignant potential.
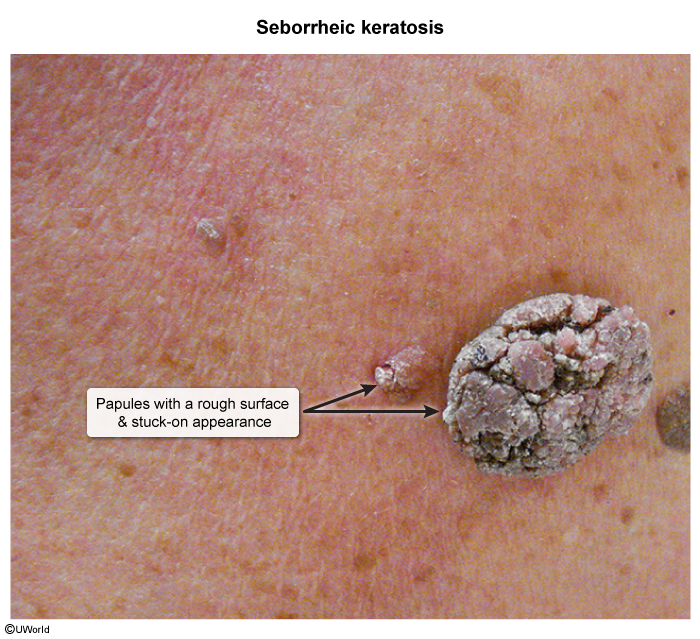 image 8
image 8 - Atopic dermatitis: When chronic, presents with scaly papules ( and lichenified plaques. Unlike AK, atopic dermatitis is significantly pruritic and typically has an onset in childhood.
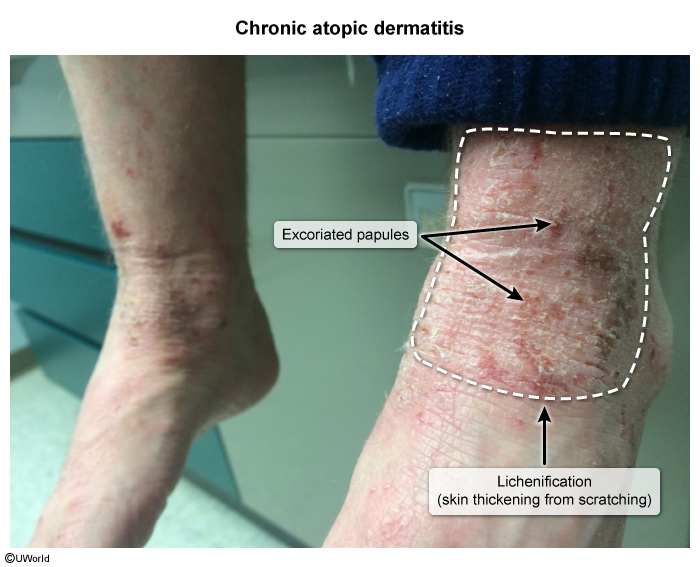 image 9
image 9 - Keratoacanthoma: Grows rapidly over 6-8 weeks from a macule to a papule to a well-circumscribed nodule with a central keratinous core ( It is thought that keratoacanthoma may resemble or transform into SCC; however, it is clinically distinct from AK.
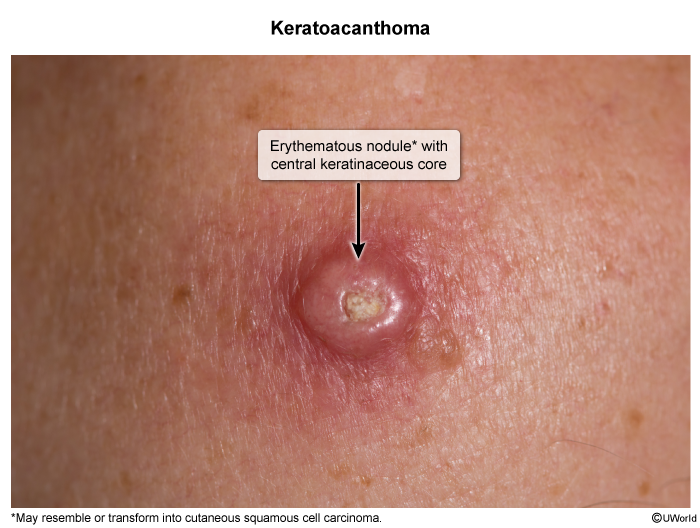 image 10
image 10 - Melanoma: Usually presents as asymmetric, pigmented macules or nodules, often with irregular borders and color variegation. Lentigo maligna (melanoma in situ) ( can mimic pigmented AK, but histologic examination typically shows melanocytic proliferation and atypia, not keratinocyte proliferation and atypia as seen in AK.
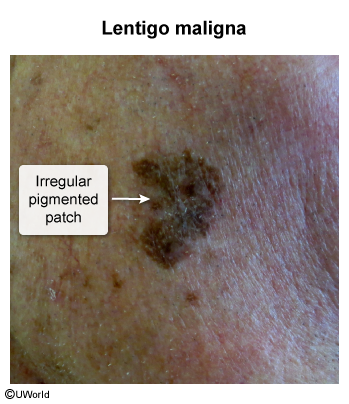 image 11
image 11 - Basal cell carcinoma: Among the most common types of skin cancer; often presents as a pearly papule with rolled borders and/or intralesional telangiectasia ( It typically does not have a scaly appearance, unlike AK.
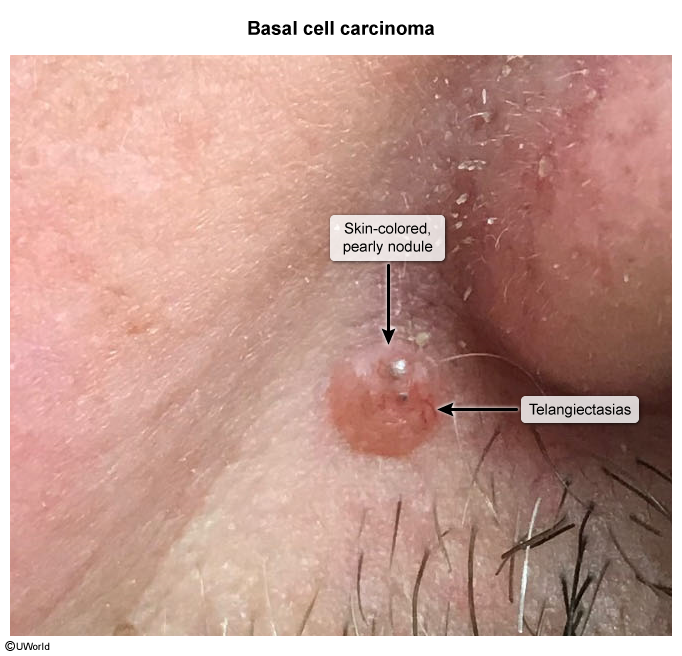 image 12
image 12 - Psoriasis: Commonly presents as erythematous plaques with thick silvery scales. Unlike hypertrophic AK, psoriatic plaques ( are typically larger and symmetrical, occurring on bilateral extensor surfaces (eg, knees, elbows).
 image 13
image 13 - Solar lentigines: Also known as age spots or liver spots. Benign, asymptomatic, pigmented macules ( that appear in fair-skinned individuals on sun-exposed areas of the skin. Unlike AK, they do not have scales.
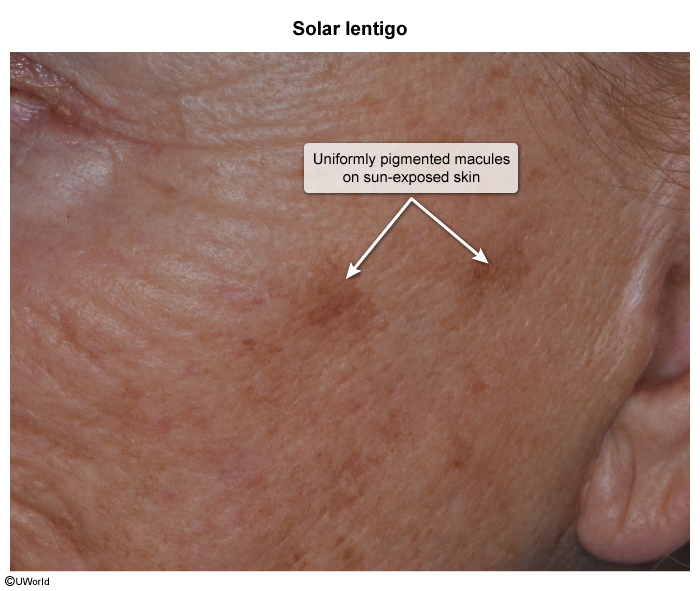 image 14
image 14
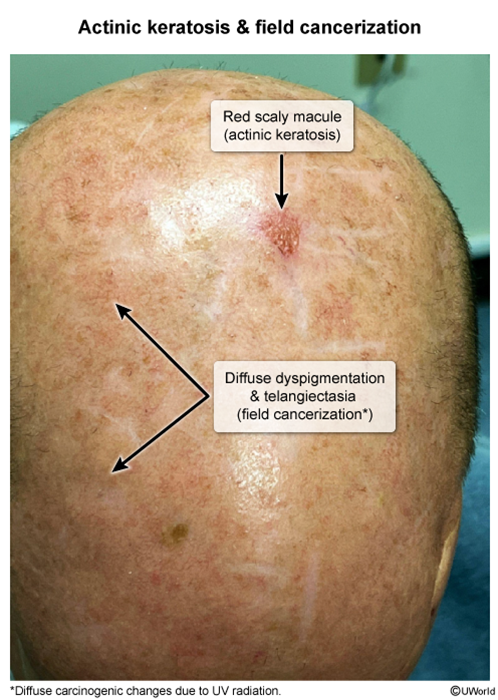
Management
Management of AK depends on the extent of the lesions.
- Few, isolated AKs can generally be treated effectively with liquid nitrogen cryotherapy.
- In contrast, widespread AKs and field cancerization should be treated with topical chemotherapy (eg, 5-fluorouracil, imiquimod, tirbanibulin) because the cream can easily be applied to cover the entire affected area.
In addition, every patient with AK should be advised on prevention (eg, sunblock, avoidance of sun exposure, protective clothing) and surveillance (eg, periodic skin examinations) measures.
Prognosis
AKs can regress, persist as AK, or transform to SCC.
- Malignant transformation rate: <1-3% per year.
- Regression rate: 20%-30% per year.
Transformation of AK into SCC is reflected in an increase in lesion size and thickness (therefore, lesions ≥1 cm or lesions that are indurated require biopsy to rule out SCC).
Summary
Actinic keratosis (AK
is a common precancerous skin lesion that may progress to cutaneous squamous cell carcinoma (SCC). They arise as a result of keratinocyte mutations induced by ultraviolet radiation exposure (ie, chronic sun exposure). AKs typically present as erythematous scaly papules with a sandpaper-like texture on sun-exposed areas (eg, face, ears, dorsal hands). A background of photodamaged skin exhibiting dyspigmentation, rough texture, atrophy, and/or telangiectasia often exists, features indicative of cellular carcinogenic changes; this clinical presentation is called field cancerization.Diagnosis is primarily clinical, but a biopsy should be performed to confirm the diagnosis when suspicion for SCC is high (eg, indurated lesions, lesions ≥1 cm). The goal of treatment is to prevent progression to SCC. Isolated AKs can be treated with liquid nitrogen; field cancerization or widespread AKs can be treated with topical chemotherapeutic agents (eg, 5-fluorouracil, imiquimod, tirbanibulin).