To see contributor disclosures related to this article, click on this reference: [1].
Physicians can earn CME/MOC credit by using this article to address a clinical question and completing a brief evaluation about how they applied the information in their practice.
AMBOSS designates this internet point-of-care activity for a maximum of 0.5 AMA PRA Category 1 Credit(s)™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
For answers to questions about AMBOSS CME, including how to redeem CME/MOC credit, see "Tips and links" at the bottom of this article.
An asthma exacerbation is the acute or subacute worsening of asthma symptoms resulting from reversible lower airway obstruction in response to a trigger (e.g., upper respiratory tract infection, allergens, medication nonadherence). The diagnosis is usually clinical and involves early evaluation of the severity of asthma exacerbation based on peak expiratory flow (PEF), oxygen saturation, and/or physical examination findings (e.g., use of accessory muscles of breathing). Additional diagnostic studies can include arterial blood gas analysis (ABG) and chest x-ray (CXR) depending on initial severity and response to treatment. Immediate treatment is essential as asthma exacerbations can be life-threatening and may progress to respiratory arrest. Treatment includes oxygen therapy, short-acting bronchodilators, i.e., short-acting beta agonists (SABA) and short-acting muscarinic antagonists (SAMA), and systemic glucocorticoids. See “Asthma" for details on long-term management.
The information in this article applies to patients older than 5 years of age.
The definitions listed here are for patients older than 5 years of age.
- Asthma exacerbation: a typically reversible episode of lower airway obstruction (bronchospasm) characterized by a worsening of asthma symptoms within a short period of time (acute or subacute) and accompanied by a change in baseline lung function [2]
- Bronchospasm: a constriction in the bronchial muscles that results in airway obstruction within seconds to minutes. It is the characteristic symptom of asthma exacerbations, but it may also be triggered by certain medications or mechanical ventilation.
- Status asthmaticus: a term used to describe severe asthma exacerbations that progress rapidly and do not respond to standard acute asthma therapy [3]
Risk factors for asthma exacerbations [2]
Uncontrolled asthma symptoms significantly increase the risk of exacerbations. The additional factors listed below increase risk regardless of whether symptoms are well controlled.
- Exposure to asthma triggers
- SABA-only treatment and/or overuse of SABA
- Inadequate inhaled corticosteroid (ICS) prescription and/or poor adherence to ICS
- Incorrect inhaler technique
- Prior intubation or ICU admission for asthma
- ≥ 1 severe exacerbations in the previous year [2]
- FEV1 < 60% of predicted average value [2]
- High bronchodilator responsiveness [2]
- Blood eosinophilia
Risk factors for fatal or near-fatal asthma exacerbations [2][4]
Near-fatal episodes include those requiring intubation and/or ICU admission.
-
Exacerbation history
- History of ≥ 1 near-fatal asthma episodes
- Hospital admission or emergency department visit for asthma exacerbation within the past year
-
Medication-related factors
- Current or recent use of oral glucocorticoids
- No current use of or poor adherence to ICS
- Heavy reliance on SABA, e.g., ≥ 200 doses used per month [2]
-
Comorbidities
- Pneumonia, cardiac arrhythmias
- Psychiatric disorders
- Diabetes mellitus
- Food allergies
- Social risk: e.g., isolation, precarious employment
Signs and symptoms vary depending on the severity of asthma exacerbation. For some individuals, an acute exacerbation may be the first manifestation of asthma. [2][3]
-
Common symptoms
- Dyspnea
- Increased coughing
-
Vital signs and general appearance
- Tachypnea
- Tachycardia
- Pulsus paradoxus [4]
- Hypoxemia (SpO2 < 90% on ambient air, possible cyanosis)
- Altered mental status
-
Signs of bronchoconstriction
- Prolonged expiratory phase
- Expiratory wheezing
- Silent chest
- Hyperresonance on percussion
- Inferior displacement and poor movement of the diaphragm
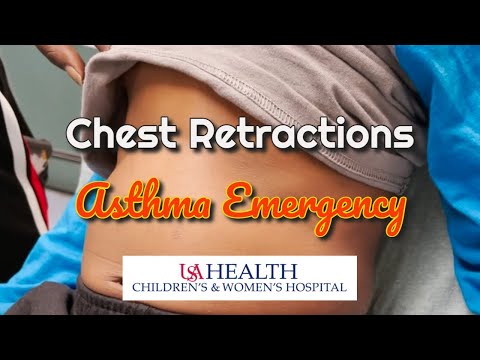
- Signs of increased work of breathing: (WOB): e.g., use of accessory muscles
Characteristic features of imminent respiratory arrest include silent chest, altered mental status, bradycardia, paradoxical breathing, respiratory muscle exhaustion, and signs of respiratory failure on ABG (e.g., normalization of pH and PaCO2 in a fatiguing patient). [5]
Crackles on auscultation are rare in asthma exacerbations and may indicate a viral or bacterial trigger (e.g., pneumonia). [5]
Acute asthma exacerbation is a clinical diagnosis based on the worsening of asthma symptoms and lung function from an individual's baseline.
Approach [2]
- Classify asthma exacerbation severity based on clinical features and measurements of SpO2 and PEF or FEV1.
- Consider additional diagnostic tests (e.g., ABG, CXR) after stabilization to:
- Evaluate for underlying causes.
- Rule out differential diagnoses (e.g., COPD, acute heart failure).
- Patients with suspected viral trigger: Start isolation precautions in accordance with local protocols.
Patients with severe or life-threatening asthma exacerbations require aggressive therapy. Do not delay immediate stabilization for diagnostic testing.
Early recognition of hypercapnic respiratory failure and/or hypoxemic respiratory failure is vital.
PFTs [2]
PFTs may not be feasible in children or in patients with a life-threatening asthma exacerbation.
-
Uses
- Stable patients: Assess severity before initiating treatment.
- All patients: Monitor response to treatment.
-
Modalities
- Peak flow meter (PFM): measures PEF, easy to obtain in exacerbations
- Spirometry: more reliable measurement, may not be feasible during exacerbations
-
Interpretation
- Compare PEF and/or FEV1 with previous personal best (preferred) or predicted average values
- PEF < 60% of predicted value is consistent with severe asthma exacerbation. [2]
- See also “Severity assessment in asthma exacerbation.”
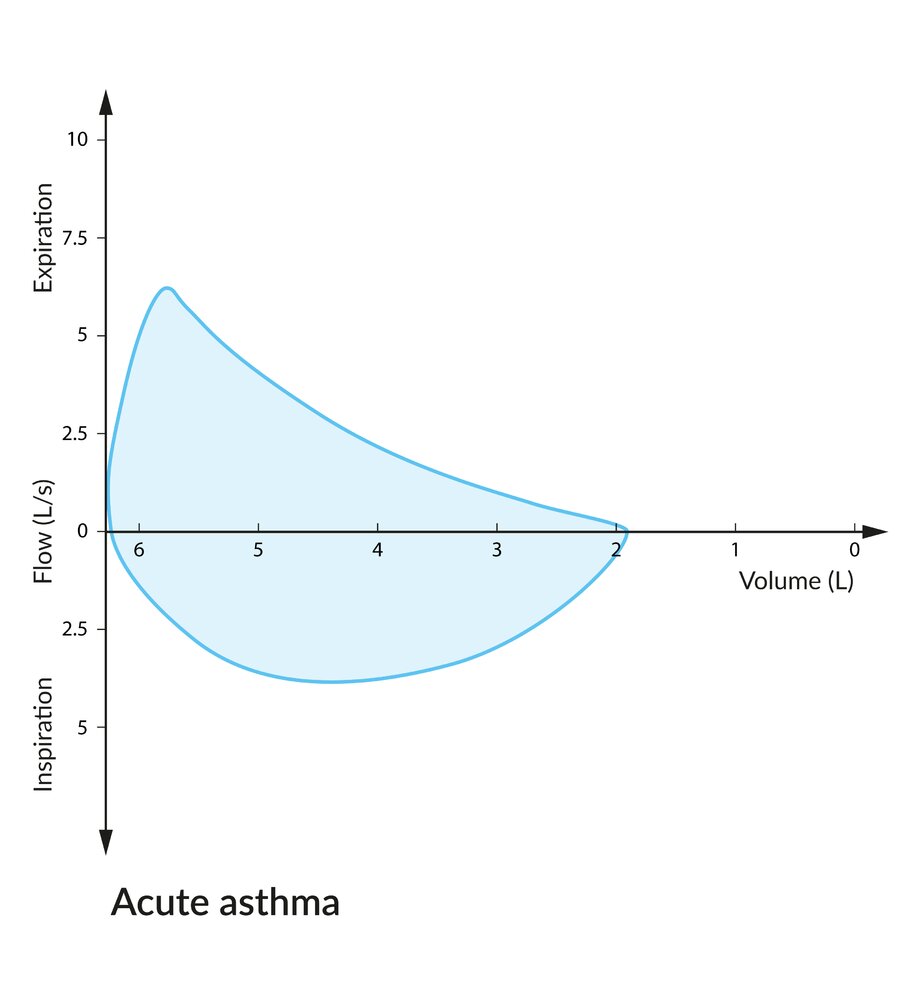
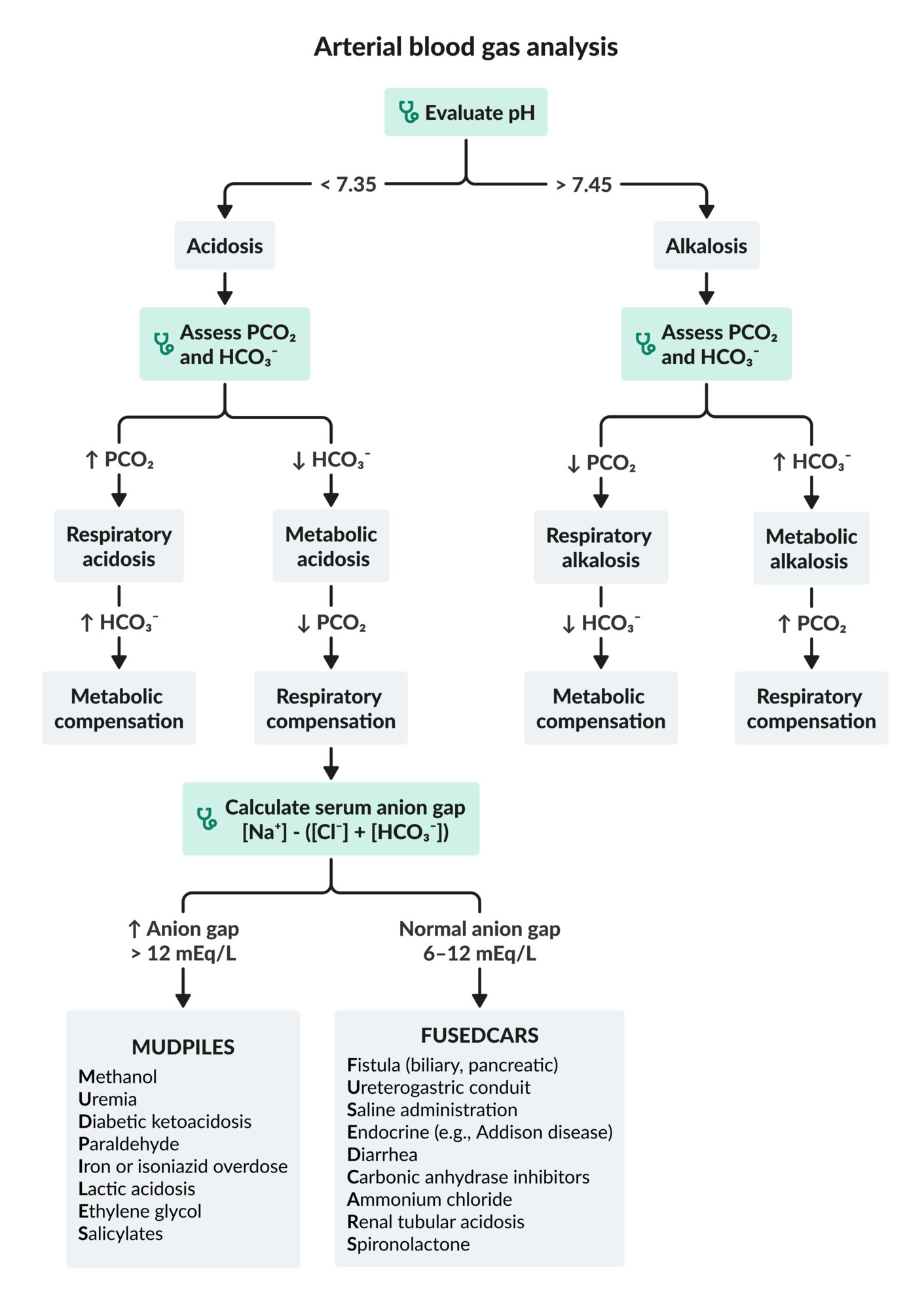
ABG [2]
Obtain ABG without interrupting supplemental oxygen administration. [2]
-
Indications
- PEF or FEV1 < 50% of the predicted average value [2]
- Clinical worsening or poor response to acute asthma therapy
-
Initial findings
- Respiratory alkalosis
- Hypoxemia may be present.
-
Late findings (indicate severe exacerbation and respiratory failure)
- Respiratory acidosis
- Severe hypoxemia (PaO2 < 60 mm Hg) [2]
- Hypercapnia (PaCO2 > 45 mm Hg) [2]
Patients with acute asthma exacerbations initially present with hypocapnia (↓ PaCO2) and respiratory alkalosis (↑ pH) due to tachypnea. Rising PaCO2 and normalizing pH in a patient with respiratory muscle fatigue are signs of impending respiratory failure!
Chest x-ray [2]
Chest x-rays are not routinely recommended. [2]
-
Indications
- Suspected comorbidity (e.g., pneumonia, pneumothorax)
- Evaluation of differential diagnoses (e.g., ARDS, CHF, foreign body aspiration)
- Lack of improvement with treatment
-
Supportive findings [6]
-
Signs of pulmonary hyperinflation
- Horizontal appearance of ribs
- Increased number of ribs above diaphragm level
- Flat diaphragm
- Bronchial thickening
-
Signs of pulmonary hyperinflation
Additional diagnostic studies [4]
-
Laboratory studies
- CBC: Consider when concomitant pneumonia is suspected.
- BMP: Consider in patients already being treated with SABAs and/or glucocorticoids.
-
Consider baseline ECG in:
- Patients > 50 years of age [4]
- Patients with COPD-asthma overlap and/or cardiovascular comorbidities (e.g., coronary artery disease)
In patients with acute asthma, evaluate for complications, such as pneumonia, atelectasis, or pneumothorax.
The following conditions manifest as sudden dyspnea with or without altered breath sounds. [7]
- AECOPD
- Anaphylaxis
- Acute bronchitis
- Foreign body aspiration
- Pulmonary embolism
- Pneumothorax
- Pneumonia
- Acute heart failure
- Sudden tracheal or bronchial compression
- Allergic bronchopulmonary aspergillosis
- Vocal cord dysfunction
- Dysfunctional breathing disorder (e.g., hyperventilation, thoracic dominant breathing) [8]
-
Specific to infants or young children
- Bronchiolitis (children < 2 years old; caused by RSV)
- Laryngotracheomalacia (infants; causes inspiratory stridor)
- Bronchopulmonary dysplasia (in premature infants)
- See also “Wheezing in children.”
- Croup
- See also “Differential diagnosis of dyspnea.”
The differential diagnoses listed here are not exhaustive.
- Severity is determined by the most severe clinical feature or functional assessment parameter. [2]
- The following severity assessment score for acute exacerbation is based on the 2025 GINA guidelines. [2][4]
- Pediatric assessment: Specific severity assessment scores for acute exacerbation of asthma in children can be used to determine disposition and guide treatment decisions.
| Classification of asthma exacerbation severity [2] | ||
|---|---|---|
| Severity | Clinical features | Functional assessment parameters |
| Mild or moderate asthma exacerbation |
|
|
| Severe asthma exacerbation |
|
|
| Life-threatening asthma exacerbation |
|
|

Management is given according to asthma exacerbation severity and continuously adjusted as needed.
Approach [2][4]
-
Severe to life-threatening asthma exacerbation
- Urgent respiratory support
- Supplemental oxygen therapy
- Prepare for intubation and mechanical ventilation in asthma (i.e., have equipment and induction agents ready).
- Monitor for signs of impending respiratory failure.
-
Maximize pharmacotherapy for acute asthma exacerbations.
- NebulizedSABA
- Plus nebulizedSAMA
- Plus oral or IVglucocorticoids
- Consider a single dose of IV magnesium sulfate.
- Consider ICS-containing therapy.
- Consider fluid repletion (preferably oral) in infants and young children.
- Urgent respiratory support
-
Mild to moderate exacerbation
- Supplemental oxygen therapy
- Pharmacotherapy
- Inhaled SABA
- Consider inhaled SAMA
- Plus oral corticosteroids
Intubation should not be delayed once an indication to intubate in asthma is identified. [4]
ASTHMA: Albuterol, STeroids, Humidified O2, Magnesium (severe exacerbations), and Anticholinergics (ipratropium bromide) are the therapies for asthma exacerbations.
Pharmacotherapy for acute asthma exacerbation
Bronchodilators [2][4]
Use a nebulizer when administration via metered-dose inhaler (MDI) with a spacer is not possible [4]
-
Inhaled SABA
- Indication: all patients
-
Preferred agent
- Albuterol MDI (off-label) with a spacer [2]
- OR nebulized albuterol (off-label) [4]
- Onset of action: < 5 minutes
- Significant clinical improvement is typically expected within the first hour of treatment.
-
Inhaled SAMA
- Indications [2]
- All patients with severe asthma exacerbation [2]
- May be considered in patients with mild or moderate exacerbation
- Agent: ipratropium bromide MDI (off-label) OR nebulized ipratropium bromide (off-label) [4]
- Onset of action: ∼15 minutes
- Indications [2]
-
ICS-containing therapy [2]
- Indication: Consider for all patients.
- Agents
- ICS/LABA, e.g., budesonide/formoterol
- ICS: budesonide, mometasone, beclomethasone
- Dosage
- Usual dosage should be increased for 2–4 weeks [2]
- See “Overview of commonly used asthma medications” for suggested dosages.
Frequent administration of an inhaled SABA is the treatment of choice to reverse airway obstruction caused by bronchospasm. [2]
Systemic therapy
-
Glucocorticoids
- Indication: all patients except those with very mild exacerbations being managed on an outpatient basis
- Routes: PO preferred over IV [2]
- Agents include: prednisolone OR equivalent dosage of either prednisone OR methylprednisolone [2]
- Recommended timing of administration: within 1 hour of presentation [2]
- Onset of action: within 4 hours [2]
-
IV magnesium sulfate [2]
- Indications
- All patients with persistent hypoxemia after initial therapy
- Adults with FEV < 25–30% of predicted average value at presentation
- Children with FEV < 60% of predicted average value after 1 hour of treatment
- Dosage: IV magnesium sulfate (off-label) [2]
- Cautions: Monitor for signs of hypermagnesemia.
- Indications
Administration of glucocorticoids within 1 hour of presentation reduces the risk of inpatient admission. [9]

Additional therapies [2][4]
-
Treatment for concomitant conditions
- Anaphylaxis: Combine treatment with epinephrine; see “Management of anaphylaxis” for details. [5]
- Pneumonia: Initiate antibiotic therapy; see “Treatment of pneumonia” for details.
-
Advanced therapies: Consider only under specialist guidance.
- Continuous SABA nebulizer [2]
- Helium oxygen therapy (heliox) [2][10]
- IV beta-2 agonists [2]
- IV leukotriene-receptor antagonists
The following therapies should be avoided because their benefits are limited and outweighed by risks and side effects: theophylline, aminophylline, mucolytics, sedatives, and chest physiotherapy. [4]
Oxygen therapy in asthma [2]
- Provide controlled oxygen therapy (e.g., via Venturi mask).
- Titrate as needed to attain target SpO2: [2]
- Individuals aged ≥ 12 years: 93–95% [2]
- Children aged 6–11 years: ≥ 94% [2][11]
Administration of 100% oxygen therapy in patients with severe exacerbations is associated with worse clinical outcomes than controlled low-flow oxygen therapy. [2]
Intubation [4][10]
-
Indications for intubation in asthma include: [10]
- Cardiac and/or respiratory arrest
- Life-threatening asthma exacerbation that does not respond to initial medical therapy
-
Imminent respiratory arrest despite maximal treatment, as evidenced by:
- Persistent or worsening hypoxia and/or hypercapnia
- Respiratory acidosis
- Worsening mental status
- Experienced clinical judgment: based on a multifactorial estimate of the likelihood of progression to respiratory failure
-
Associated risks
- Worsening of bronchospasm
- Increased peri-intubation mortality
- Hypoxic brain injury
- Cardiac arrest
- Circulatory collapse
-
Recommendations
- Administer intubation induction agent, e.g., ketamine (preferred) ; see “Intubation medications” for more details. [12]
- See “High-risk indications for mechanical ventilation” for peri-intubation risk reduction.
Mechanical ventilation
-
Invasive mechanical ventilation
- Start mechanical ventilation with 100% oxygen using a ventilation strategy for obstructive lung disease.
- Permissive hypercapnia is typically applied to prevent ventilator-induced lung injury (e.g., barotrauma).
- Continue bronchodilator therapy via ventilator tubing once patient is mechanically ventilated.
- See “Troubleshooting of mechanical ventilation” for strategies to optimize gas exchange and management of complications (e.g., hemodynamic impairment, dynamic hyperinflation).
-
Noninvasive positive-pressure ventilation (NIPPV)
- Can be used as a bridge to intubation
- May be more effective for preoxygenation than a nonrebreather mask
- Consult a critical care specialist if considering NIPPV.
- There is insufficient evidence for using NIPPV to prevent intubation.
- Can be used as a bridge to intubation
Intubation and mechanical ventilation are challenging, high-risk procedures that should be performed by an experienced practitioner whenever possible.
Monitoring [2][4]
-
Assess response to initial therapies [2][4]
- Perform serial examinations to assess symptom severity and physical examination findings.
- Frequently monitor vital signs, O2 saturation, and PaCO2 levels.
- Measure pulmonary function after an hour of initial treatment.
-
Adjust treatment based on response to therapy
- Evaluate post-treatment parameters to determine disposition and guide further treatment decisions.
- Escalate treatment in patients with a poor or incomplete response to acute asthma therapy.
Consider continuous cardiac and pulse oximetry monitoring in patients with risk factors for fatal or near-fatal asthma exacerbations.
Response to initial therapy [2][4]
| Response to initial therapy in acute asthma exacerbations [4] | |
|---|---|
| Poor response to acute asthma therapy |
|
| Incomplete response to acute asthma therapy |
|
| Good response to acute asthma therapy |
|
Disposition
Disposition in acute asthma is determined by the severity of asthma exacerbation at presentation as well as the response to initial therapy. [2][4]
-
ICU admission
- Life-threatening asthma at presentation
- Any severity with poor response to acute asthma therapy
-
Acute care settings
- Mild, moderate, or severe asthma exacerbation at presentation with either:
- Risk factors for fatal or near-fatal asthma
- Incomplete response to acute asthma therapy
- Mild, moderate, or severe asthma exacerbation at presentation with either:
-
Outpatient management
- Consider when all of the following parameters are met:
- Mild or moderate asthma exacerbation at presentation
- Good response to acute asthma therapy sustained for ≥ 60 minutes
- Ability to complete treatment at home
- Recommend follow-up in 2–7 days or earlier if symptoms recur.
- Consider when all of the following parameters are met:
See “Disposition in acute asthma” for indications for outpatient management.
Pharmacotherapy [2]
- Continue SABA (e.g., albuterol) for symptom control.
- Resume or initiate ICS/formoterol for maintenance and reliever therapy (see “Asthma management” for doses). [2]
- Continue systemic glucocorticoids (if started) in: [2][4]
- Adults: typically 5–7 days
- Children: typically 3–5 days
Patient education [2]
Provide patient education according to the care setting.
- Review and/or teach inhaler technique.
- Emphasize the importance of using a spacer with an MDI.
- Teach the patient how to use a PFM and how to record and interpret PEF measurements.
- Advise the patient to identify and avoid asthma triggers whenever possible.
- Review symptom recognition and reasons to seek care (e.g., increased need for rescue therapy).
Provide an individualized written action plan for patients and/or caregivers.
We appreciate your feedback!
We’re testing dot phrases with ready-to-use assessment and plan templates.
Please verify all information before use; follow local protocols and procedures when available.
Acute asthma (mild to moderate)
Assessment: This is a @AGE@-year-old @SEX@ with a history of asthma presenting with [**dyspnea/chest tightness/cough/wheeze], most likely caused by a mild to moderate asthma exacerbation. Features supporting mild to moderate classification include [**able to speak in complete phrases or sentences, no agitation, no use of accessory muscles of breathing, HR ≤ 120 bpm].
Differential diagnoses: AECOPD, anaphylaxis, acute bronchitis, foreign body aspiration, PE, pneumothorax, pneumonia, acute heart failure, tracheal or bronchial compression, allergic bronchopulmonary aspergillosis, vocal cord dysfunction, dysfunctional breathing disorder (e.g., hyperventilation, thoracic dominant breathing)
Plan
Disposition
-[Admit to Medicine because the patient has risk factors for fatal or near-fatal asthma and/or incomplete response to acute asthma therapy.]
-OR [Outpatient management because all of the following parameters are met: mild or moderate asthma exacerbation at presentation, good response to acute asthma therapy sustained for ≥ 60 minutes, ability to complete treatment at home]
Monitoring and support
-Pulse oximetry
-Supplemental oxygen: Titrate to SpO2 93–95%.
Meds
[**Adults]
-Albuterol MDI 4–10 inhalations every 20 minutes for the first hour, then 4–10 inhalations every 1–4 hours PRN
-Ipratropium bromide HFA 8 inhalations every 20 minutes for up to 3 hours PRN
-Prednisolone 50 mg IV or PO once daily
[**Children]
-Albuterol MDI 4–10 inhalations every 20 minutes for the first hour, then 4–10 inhalations every 1–4 hours PRN
-Ipratropium bromide HFA (18 mcg/inhalation) 4–8 inhalations every 20 minutes for up to 3 hours PRN
-Prednisolone 1–2 mg/kg IV or PO once daily
Follow up with PCP in 2–7 days or earlier if symptoms recur.
Acute asthma (severe to life-threatening)
Assessment: This is a @AGE@-year-old @SEX@ with a history of asthma presenting with [**dyspnea/chest tightness/cough/ wheeze], most likely caused by a severe/life-threatening asthma exacerbation. Features supporting severe classification include [**unable to speak in complete phrases or sentences, tripod position, agitation, use of accessory muscles of breathing, respiratory rate > 30 breaths/minute, HR > 120 bpm.] Features supporting life-threatening classification include [**drowsiness, confusion, silent chest (absence of wheezing), unable to speak due to dyspnea, paradoxical breathing, bradycardia].
Differential diagnoses: AECOPD, anaphylaxis, acute bronchitis, foreign body aspiration, PE, pneumothorax, pneumonia, acute heart failure, tracheal or bronchial compression, allergic bronchopulmonary aspergillosis, vocal cord dysfunction, dysfunctional breathing disorder (e.g., hyperventilation, thoracic dominant breathing)
Plan
Disposition
-Admit to ICU for [**life-threatening asthma at presentation] and/or [**PEF < 40% of predicted average value, PaCO2 ≥ 42 mm Hg, ≥ 1 symptoms of severe asthma exacerbation; drowsiness and/or confusion] after initial therapy.
–OR Admit to Medicine/Pediatrics for [**risk factors for fatal or near-fatal asthma] and/or [**incomplete response to acute asthma therapy].
Urgent respiratory support
–Consult anesthesia, respiratory therapy, and critical care [if there are indications for intubation: **cardiac and/or respiratory arrest, life-threatening exacerbation not responsive to initial medical therapy, imminent respiratory arrest]
–Supplemental oxygen: Titrate to SpO2 93–95%.
Meds
[**Adults]
–Albuterol 2.5–5 mg nebulized every 20 minutes for up to 3 doses, then 2.5–10 mg every 1–4 hours PRN
–Ipratropium bromide 0.5 mg nebulized every 20 minutes for 1 hour; continue PRN.
–Prednisolone 50 mg IV/PO once daily
–Magnesium sulfate 2 g IV over 20 minutes
[**Children]
–Albuterol 0.15 mg/kg nebulized every 20 minutes for up to 3 doses, then 0.15–0.3 mg every 1–4 hours PRN (min. single dose 2.5 mg; max. single dose 10 mg)
–Ipratropium bromide 0.25–0.5 mg nebulized every 20 minutes for 1 hour; continue PRN.
–Prednisolone 1–2 mg/kg IV or PO once daily (max. dose 40 mg/day)
- Perform ABCDE survey.
- Assess severity of asthma exacerbation (clinical evaluation, PEF).
- Administer pharmacotherapy, e.g., inhaled SABA PLUS inhaled SAMA PLUS IV glucocorticoids.
- Titrate oxygen therapy to target SpO2, i.e.:
- 93–95% in individuals ≥ 12 years of age
- 94–98% in children 6–11 years of age
- For life-threatening asthma exacerbations:
- Consult critical care.
- Consider adjunctive therapies to prevent intubation (e.g., magnesium sulfate).
- Intubate early if indications for intubation in asthma are identified.
- Use ventilation strategy for obstructive lung disease.
- Reassess severity frequently and escalate treatment as needed.
Acute asthma exacerbation during pregnancy [2]
-
Epidemiology
- Approx. one third of individuals with asthma experience a worsening of symptoms during pregnancy. [2]
- Exacerbations typically occur in the second trimester.
- Etiology: anatomical and/or hormonal changes, reduction or cessation of medications (e.g., ICS), viral respiratory infections
-
Risk factors [2]
- Severe asthma
- Multiparity
- Current smoking
- Age > 35 years
- Obesity
- Depression and/or anxiety
-
Management
- Treat exacerbations aggressively with SABAs, supplemental oxygen, and systemic glucocorticoids; see “Pharmacotherapy for acute asthma exacerbations” for dosages.
- Monitor neonatal blood glucose levels for 24 hours if high doses of SABAs have been given within 48 hours of delivery. [2]
-
Complications
- Preterm delivery
- Low birth weight
- Preeclampsia
-
Prevention
- Provide usual asthma maintenance medications during labor and delivery.
- Avoid de-escalating or stopping ICS-containing therapy shortly before or during pregnancy.