Acute chest syndrome (ACS) is a potentially fatal complication of sickle cell anemia caused by vaso-occlusion of the pulmonary vasculature. Symptoms may include chest pain, shortness of breath, and fever. Diagnosis is based on clinical symptoms and chest imaging findings of a new pulmonary infiltrate. Management consists of antibiotics, supportive care with IV fluids and oxygen, and possibly a blood transfusion.
See also “Sickle cell disease.”
- Vaso-occlusion of the pulmonary vasculature
- Triggers include infection, asthma, surgery/general anesthesia
- Common cause of death in patients with sickle cell disease [1]
- Chest pain
- Fever
- Respiratory distress, cough, shortness of breath, wheezing
- Signs of vaso-occlusive crisis (e.g., pain in arms or legs)
- Rib or sternal pain
- See also “Complications” below.
ACS is a clinical diagnosis supported by characteristic clinical features and the presence of new pulmonary infiltrate on imaging. [1]
Diagnostic criteria for acute chest syndrome [2][3][4]
- Clinical findings of one or more of the following:
- Chest pain
- Cough
- Temperature > 38.5°C
- Tachypnea
- Hypoxemia
- Signs of increased work of breathing
- Wheezing
- Crackles
- PLUS a new pulmonary infiltrate on CXR that involves at least one lung segment and is not due to atelectasis [4]
Laboratory studies
-
Routine
- CBC: anemia, leukocytosis, thrombocytopenia [5]
- Type and screen and crossmatch
-
BMP and LFTs: signs of multiorgan failure may be present
- Elevated creatinine
- Elevated AST and ALT
- Sputum and blood cultures [6]
- Arterial blood gas: Gold standard for determining partial pressure of oxygen and carbon dioxide [7]
-
Additional
- Consider PCR for viral panel and serologies for respiratory pathogens (e.g., Mycoplasma, Legionella): See pneumonia diagnostics.
- Consider troponin to assess for myocardial injury.
Imaging
-
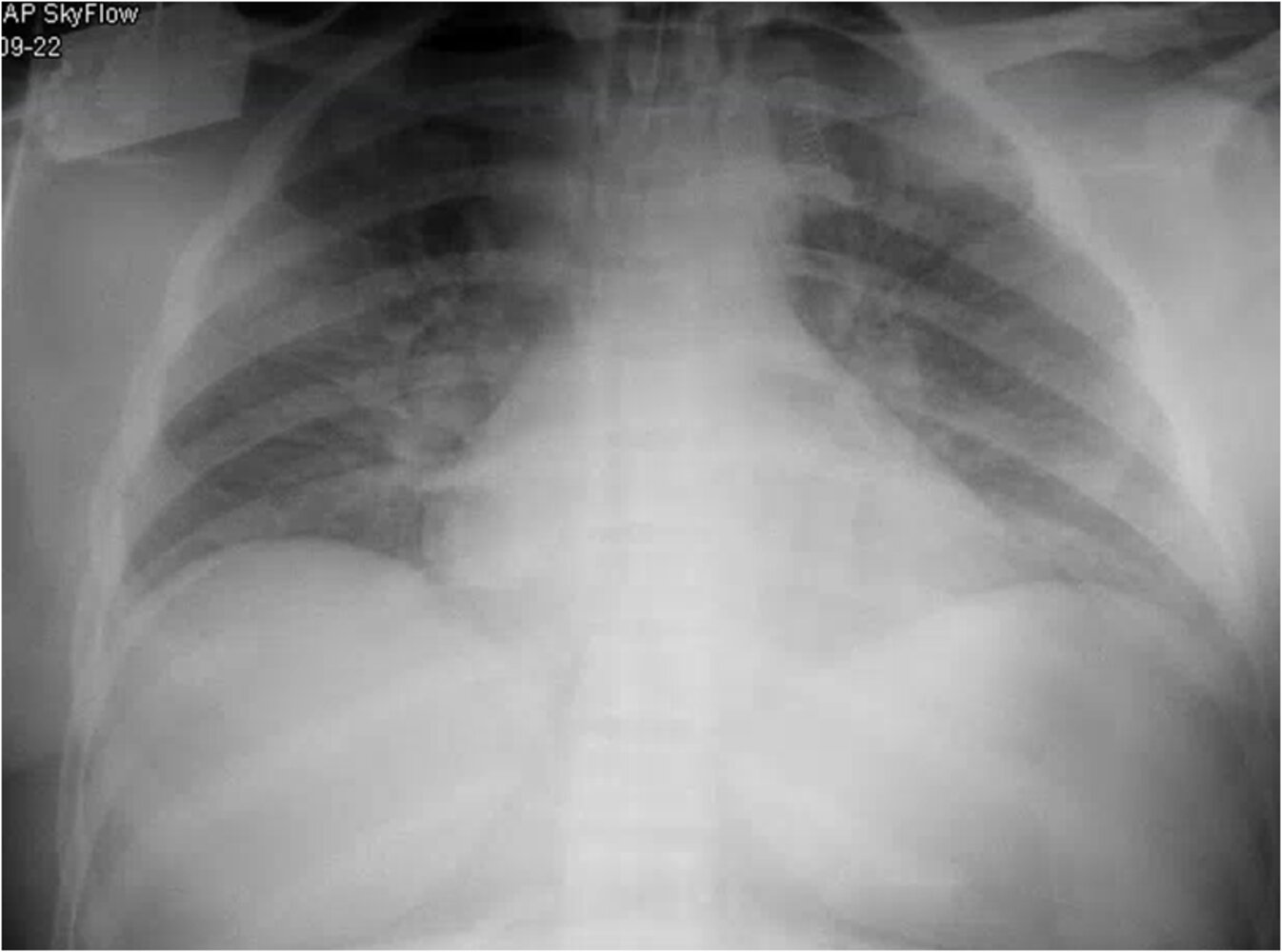
Chest x-ray
- Indication: all patients suspected of having ACS
- Supportive findings:
- New pulmonary infiltrate
- Segmental, lobar, or multilobular consolidation with or without the presence of pleural effusion
- If CXR is normal, it should be repeated in 24–48 hours if there is ongoing clinical suspicion for ACS. [6]
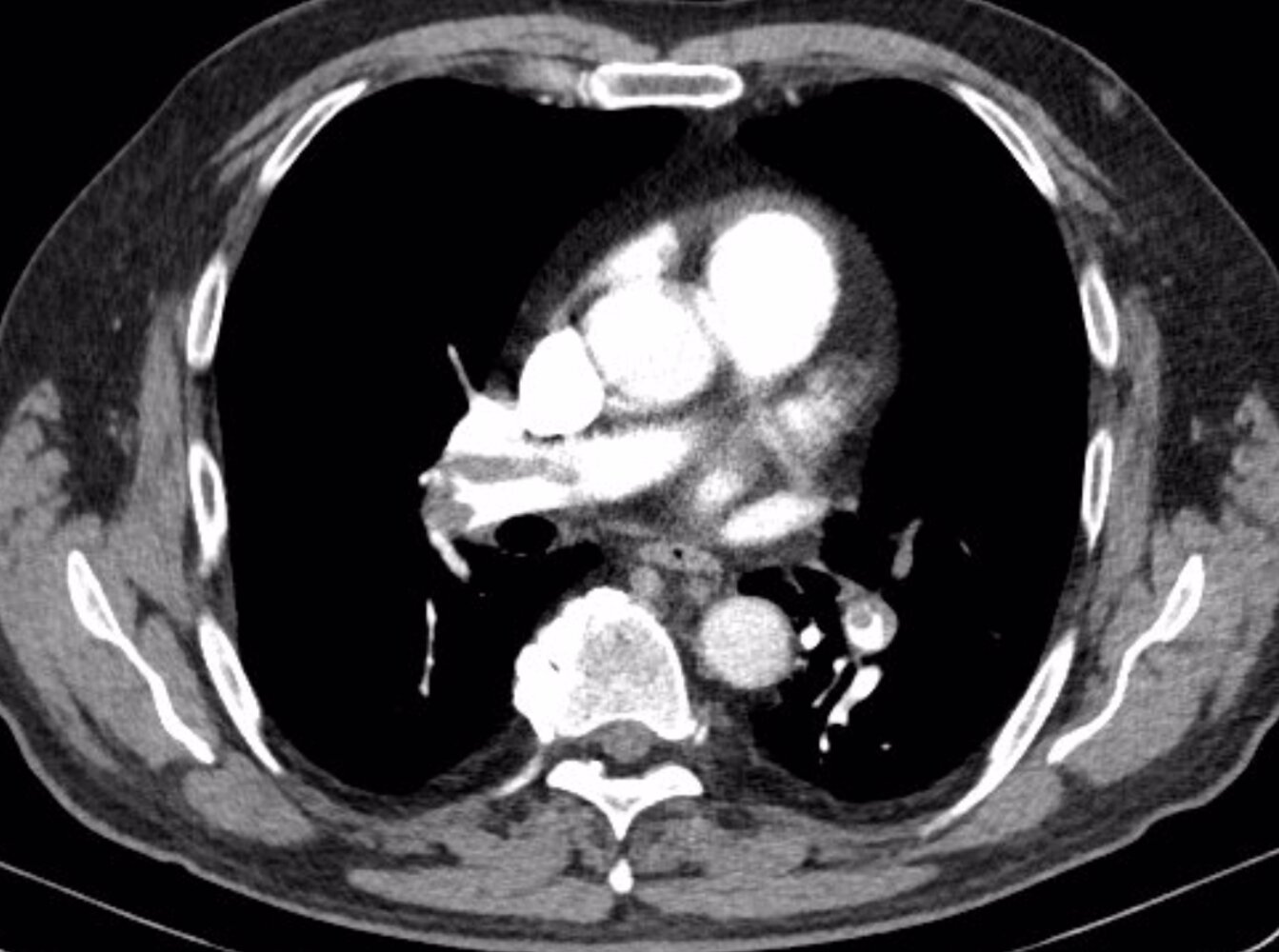
- CT pulmonary angiography: if there is a concern for pulmonary embolism (PE) [8]
Other
- ECG: Assess for acute myocardial injury (see diagnosis of myocardial infarction).
- Bronchoscopy with bronchoalveolar lavage: performed in refractory cases and/or in atypical presentations for assessment of viral or bacterial causes
General principles [1][4][9]
-
All patients
- Supportive care
- Antibiotics
- Evaluation for blood transfusion
- Hospital admission with close monitoring and hematology consult
-
Critically ill or rapidly progressing patients
- Respiratory and hemodynamic support
- Evaluation for urgent exchange transfusion
- Admission to the ICU
-
Patients with recurrent ACS
- Allogenic stem cell transplantation may be indicated.
- See “Long-term management of sickle cell disease”. [10]
Supportive care
-
Respiratory support
- Supplemental oxygen: target SpO2 > 95%
- Identify patients at risk of progression to respiratory failure. [1]
- PaO2 ≤ 60 mm Hg
- Opioid-induced respiratory depression
- Features of impending severe ACS (see “Monitoring”)
- Initiate NIPPV or invasive mechanical ventilation as needed (see mechanical ventilation and management of ARDS). [1]
-
Additional supportive care
- Pain management: opioids administered as scheduled doses or continuous infusion via patient-controlled analgesia
-
IV fluids: Avoid overhydration, which can lead to pulmonary edema. [7]
- For patients with hypovolemia: cautious use of normal saline bolus [11]
- The choice of fluids depends on hydration status.
- Isotonic fluids are recommended for urgent volume correction.
- Hypotonic fluids are recommended otherwise, i.e., 5% dextrose in either water, 0.45% normal saline, or 0.22% normal saline.
- Recommended rate: no greater than 1.5 times the maintenance fluid requirement
- Bronchodilators (e.g., albuterol): especially in patients with a history of asthma or evidence of acute bronchospasm
- Incentive spirometry to prevent atelectasis
- VTE prophylaxis [1]
- Treatment of associated complications: See “Complications.”
Avoid overhydration in patients with acute chest syndrome because of the risk of pulmonary edema.
Antibiotic therapy [7]
- Obtain blood cultures (two sets) and sputum cultures before starting antibiotics.
- Start empiric antibiotics (see empiric antibiotic therapy for community-acquired pneumonia).
- Suggested regimen
- A third-generation cephalosporin (e.g., ceftriaxone) [12][13]
- PLUS a macrolide (e.g., azithromycin) [4]
- Suggested regimen
Blood transfusion
-
Simple blood transfusion [4]
- pRBCs indicated if hemoglobin concentration is > 1.0 g/dL below baseline
- May not be indicated if the patient’s baseline hemoglobin is ≥ 9 g/dL
- For HbSC or HbS/β-thalassemia, consult hematology.
-
Urgent exchange transfusion [4]
- Indications
- Oxygen saturation < 90% even with supplemental oxygen
- Worsening respiratory distress
- Worsening pulmonary infiltrates
- Hemoglobin concentration continuing to decline after a simple transfusion
- Consult an apheresis specialist, if applicable.
- Consider central venous access. [14]
- Indications
Monitoring and disposition
-
Monitoring
- Continuous or frequent (e.g., every 4 hours) pulse oximetry monitoring
- Consider continuous cardiac monitoring.
- Consider frequent clinical assessments of patients with features of impending severe ACS. [4]
- Multilobe disease on chest imaging
- Pleural effusion
- Respiratory distress
- Persistent oxygen saturation < 95% despite supplemental oxygenation
- Neurological features: seizure, stroke, altered mental status
- Low platelets (< 200,000/mm3) [3]
- History of cardiac disease [3]
- Monitor for progression to multisystem organ failure.
- Monitor closely for anemia and bronchospasm.
-
Disposition
- Admit all patients to the hospital. [4]
- Admit/transfer to the ICU if the patient is at risk of progression to respiratory failure, is intubated, and/or requires an exchange transfusion.
-
Acute [1][3][7]
- Neurological: altered mental status, seizure, stroke, intracranial hemorrhage [1][3]
- Pulmonary: PE, pulmonary hemorrhage, cor pulmonale
- Splenic sequestration causing hypovolemic shock
- Multisystem organ failure
-
Chronic [1][3][7]
- Chronic sickle lung disease
- Pulmonary fibrosis
- Premature mortality
We list the most important complications. The selection is not exhaustive.
- Pain management
- IV fluids: avoid overhydration
- Blood cultures (2 sets) and sputum cultures
- Start empiric antibiotics (see empiric antibiotic therapy for community-acquired pneumonia).
- Supplemental oxygen
- Rule out alternative causes (e.g., myocardial infarction, PE).
- Hematology consultation
- Evaluate the need for transfusion and obtain type and screen.
- Bronchodilators in patients with a history of asthma or evidence of acute bronchospasm [1]
- Incentive spirometry
- Hospital admission
- Transfer to ICU if the patient is at risk of progression to respiratory failure, intubated, and/or requires an exchange transfusion.