Introduction
Acute prostatitis is an acute inflammation of the prostate gland typically caused by a bacterial infection
Risk factors
Several factors can increase the likelihood of developing acute bacterial prostatitis:
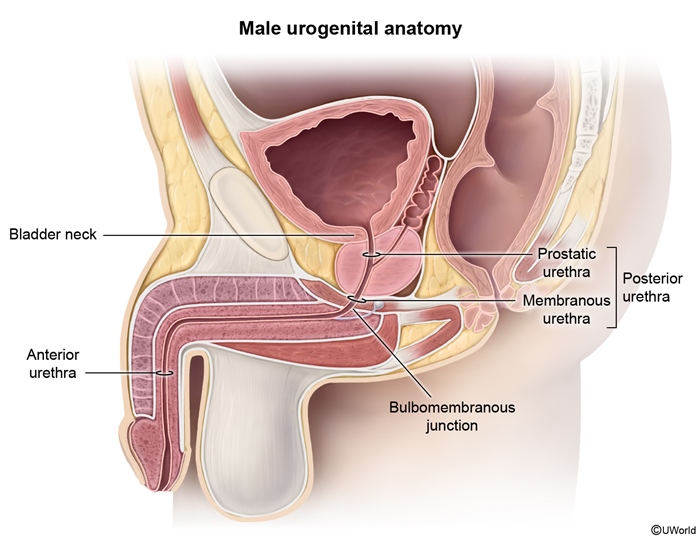
- Urogenital tract infections (eg, cystitis, urethritis): Bacteria migrate from the urethra or bladder into the prostate via urinary reflux.
- Urologic instrumentation (eg, bladder catheterization, cystoscopy): Certain procedures may inadvertently introduce bacteria into the urethra.
- Urinary retention (eg, urethral stricture, benign prostatic hyperplasia): Incomplete bladder emptying and diminished forward flow of urine increase the risk for infection and reflux.
- Unprotected sexual intercourse: This promotes entry of bacteria, including sexually transmitted infections (eg, Chlamydia trachomatis, Neisseria gonorrhoeae), into the urethra. It is more common in young men.
- Prostate biopsy/surgery: This may cause inoculation directly into the prostate.
- Immunocompromise (eg, diabetes mellitus, HIV/AIDS): This state increases susceptibility to infection.
Pathophysiology
Most cases of acute bacterial prostatitis arise when colonic pathogens contaminate the urethra and subsequently enter the sterile prostate via intraprostatic reflux of urine. E coli (a gram-negative bacillus) is the leading pathogen, causing ~75% of cases; other enteric organisms include Enterococcus faecalis, Klebsiella pneumoniae, Proteus mirabilis, and Pseudomonas aeruginosa.
Gram-positive infections (eg, Staphylococcus aureus, Streptococci) are less common and should prompt evaluation for remote infection elsewhere (eg, hematogenous spread from endocarditis).
Clinical presentation
Patients with acute prostatitis usually experience a combination of lower urinary tract symptoms and systemic symptoms:
- Lower urinary tract symptoms
- Dysuria (painful urination)
- Urinary frequency and urgency
- Pelvic, perineal, or lower back pain
- Bladder obstruction/urinary retention: Prostatic swelling can sometimes impinge the urethra and cause difficulty voiding (eg, dribbling); urinary obstruction can lead to renal insufficiency due to increased pressure on the kidney.
- Systemic symptoms include fevers, chills, malaise, and myalgia.
- Digital rectal examination shows a tender, swollen, and warm prostate. Rectal examination should be performed with care; vigorous massage can increase the risk for bacteremia.
Diagnosis
Acute bacterial prostatitis should be suspected in any patient with fever, perineal pain, and lower urinary symptoms. To establish a definitive diagnosis, digital rectal examination is required. The presence of prostatic warmth, edema, and tenderness indicates acute bacterial prostatitis.
Urinalysis with nitrites, leukocyte esterase, pyuria, and bacteriuria further supports the diagnosis; a urine culture identifies the causative organism.
Differential diagnosis
- Urinary tract infection (eg, cystitis): dysuria, frequency, and urgency are characteristic, but cystitis is not typically associated with perineal discomfort, fever, or prostate tenderness.
- Epididymitis: often presents with lower urinary tract symptoms (eg, dysuria, urgency), but patients usually have scrotal pain, swelling, and tenderness as well as a purulent urethral discharge.
- Benign prostatic hyperplasia: may cause irritative voiding symptoms, but patients typically have slowly progressive bladder outlet obstruction (eg, decreased force of stream, incomplete voiding, dribbling, nocturia) and lack systemic signs of infection.
- Urethritis: is usually caused by sexually transmitted pathogens (eg, N gonorrhoeae, C trachomatis); symptomatic cases are generally marked by dysuria and urethral discharge, not prostate tenderness.
- Chronic prostatitis/chronic pelvic pain syndrome ( : presents with pelvic and perineal pain associated with voiding symptoms (eg, frequency, urgency, hesitancy) that have been ongoing (>3 months). However, patients are generally afebrile, have little or no prostate tenderness, and have a negative urine culture. The exact etiology is unclear but suspected to be noninfectious chronic inflammation.
Laboratory evaluation
The following laboratory tests are indicated in the evaluation of acute bacterial prostatitis:
- Urinalysis: pyuria, nitrates, and bacteriuria indicates infection of the urinary tract.
- Complete blood count: typically reveals leukocytosis with bandemia.
- Urine gram stain and culture: necessary to identify causative organisms.
- Sexually transmitted infection testing: in sexually active individuals.
- Blood cultures: not always required unless there is evidence of severe sepsis (eg, hypotension).
- Basic metabolic panel: severe or prolonged urinary obstruction can cause renal dysfunction with electrolyte abnormalities.
Imaging
Imaging (eg, CT scan, prostate ultrasonography) is generally not required and should be reserved for patients who are likely to have a complication such as prostatic abscess (eg, prostatic fluctuance on digital rectal examination, failure to improve with antibiotics).
Management
The management of acute bacterial prostatitis involves initiation of empiric broad-spectrum antibiotics, typically with a fluoroquinolone or trimethoprim-sulfamethoxazole (both antibiotics have excellent coverage against enteric pathogens and achieve high prostatic tissue levels). Treatment should continue for 4-6 weeks for bacterial eradication (shorter courses may lead to chronic symptoms), and the antibiotic selection may be adjusted based on urine culture results or lack of appropriate improvement. Sexually transmitted infections should be managed with appropriate antibiotics (eg, doxycycline, ceftriaxone).
Many patients can receive outpatient treatment, but hospitalization and IV antibiotics are recommended in the following situations:
- Evidence of bacteremia/sepsis or shock
- Comorbid conditions that may increase the risk for severe infection (eg, diabetes mellitus, HIV)
- Inability to tolerate oral antibiotic treatment (eg, vomiting)
- Urinary retention (often requires suprapubic catheter placement for bladder drainage)
Hospitalized patients receiving IV antibiotics can be transitioned to oral medication and discharged once symptoms improve (eg, fever resolution).
Prognosis
With prompt and appropriate treatment, most patients with acute prostatitis recover fully. However, complications can include the following:
- Prostatic abscess: There is an increased risk for abscess in patients with diabetes mellitus and HIV; percutaneous or transurethral drainage may be required.
- Urinary retention: Suprapubic catheterization is typically used to alleviate obstruction until prostatic edema subsides (passage of urethral catheters can lead to sepsis by dislodging of bacteria from infected prostate).
- Sepsis and septic shock: These conditions can be life threatening without prompt and aggressive management (eg, IV antibiotics, pressors).
- Chronic bacterial prostatitis ( : This is characterized by repeated episodes of irritative urinary symptoms (eg, dysuria, frequency) associated with recurrent bacterial infection of the prostate (usually by the same organism). The prostate may be swollen and tender, but examination is often normal and systemic symptoms are absent. Urinalysis before and after prostatic massage reveals a >10-fold increase in bacteriuria after massage. It may be related to inadequate treatment of acute bacterial prostatitis.
Summary
Acute prostatitis
is inflammation of the prostate typically caused by colonic bacteria that enter the prostate via the urethra. It usually manifests with a flu-like illness (eg, fever, myalgia) and lower urinary tract symptoms (eg, dysuria). A tender, swollen prostate on digital rectal examination confirms the diagnosis. Urine culture is required to establish the underlying pathogen, and 4-6 weeks of empiric antibiotic treatment is necessary to eradicate the infection.