An adrenal incidentaloma is an adrenal mass that is detected on imaging conducted for reasons unrelated to adrenal conditions. Most adrenal incidentalomas are nonfunctioning (hormonally inactive) benign cortical adenomas. Approximately 20% are functional (hormonally active) and/or malignant tumors. The most important diagnostic steps are to evaluate hormonal activity using biochemical testing and the risk of malignancy using imaging (primarily CT without contrast). Nonfunctioning benign adenomas do not require treatment or routine follow-up. All patients with malignant adrenal incidentalomas (e.g., metastases, adrenocortical carcinoma) and/or functional adrenal incidentalomas (e.g., pheochromocytomas or tumors causing cortisol excess) should be managed by a multidisciplinary team and may need further diagnostic assessment. Most functioning and malignant adrenal tumors require adrenalectomy.
An adrenalincidentaloma is a clinically unapparent adrenal mass detected on imaging studies conducted for reasons unrelated to the assessment of adrenal conditions. [1][2]
Adrenal masses detected in patients being screened for hereditary syndromes or undergoing staging or follow-up for extra-adrenal cancer are not included in the definition of adrenal incidentaloma.
- Prevalence: 1–6% in adults; increases with age and peaks at 40–70 years of age [1][3]
- Nonfunctioning (hormonally inactive) benign cortical adenomas: ∼ 75% of cases [1]
- Functional and/or malignant tumors: ∼ 20% of cases [1]
The vast majority of functional (hormonally active) adrenal adenomas produce excess glucocorticoids. [4]
Epidemiological data refers to the US, unless otherwise specified.
Benign adrenal incidentalomas [2][4]
-
Adrenal adenoma (most common)
- Nonfunctioning
- Functional (e.g., mild autonomous cortisol secretion, primary hyperaldosteronism, Cushing syndrome)
- Pheochromocytoma
-
Other
- Myelolipoma or schwannoma (mesenchymal origin)
- Ganglioneuroma (neurogenic origin)
- Cyst and pseudocyst
- Hematoma and hemorrhage
Malignant adrenal incidentalomas [2][4]
- Adrenal metastases (most common)
- Adrenocortical carcinoma: functional or nonfunctioning
-
Other
- Malignant pheochromocytoma
- Sarcoma
- Lymphoma
Focused history [4][5]
- Systemic symptoms (e.g., fever, fatigue, weight loss)
- Personal and family history of:
- Endocrine disorders
- Adrenal or extra-adrenal malignancy
- Genetic syndromes associated with adrenal tumors
- Medications that can affect biochemical testing (e.g., glucocorticoids)
Focused examination [4][5]
- Signs of Cushing syndrome
- Signs of pheochromocytoma
- Signs of primary hyperaldosteronism
- Signs of hyperandrogenism (e.g., hirsutism, acne) or hyperestrogenism (e.g., gynecomastia)
- Signs of adrenal insufficiency
Patients are often asymptomatic and have normal physical examination findings because the majority of adrenal incidentalomas are nonfunctioning and benign.
The majority of adrenal incidentalomas do not require further diagnostics or management after a review of imaging and initial biochemical testing.
Management approach
- Review imaging to assess the risk of malignancy (preferably CT without contrast).
-
Obtain biochemical testing to evaluate hormonal activity.
- Dexamethasone suppression test for all patients
- Additional studies (e.g., aldosterone-to-renin ratio) based on clinical suspicion for a functional and/or malignant tumor
- Consider additional imaging and/or laboratory studies based on initial findings.
- Consult a multidisciplinary team (endocrinologist, endocrine surgeon, radiologist) for management of functional tumors or if there is suspicion for malignancy. [1][2][4]
During the initial evaluation of adrenal incidentaloma, simultaneously perform a thorough clinical evaluation, review of imaging, and biochemical studies.
Imaging [1][2][4]
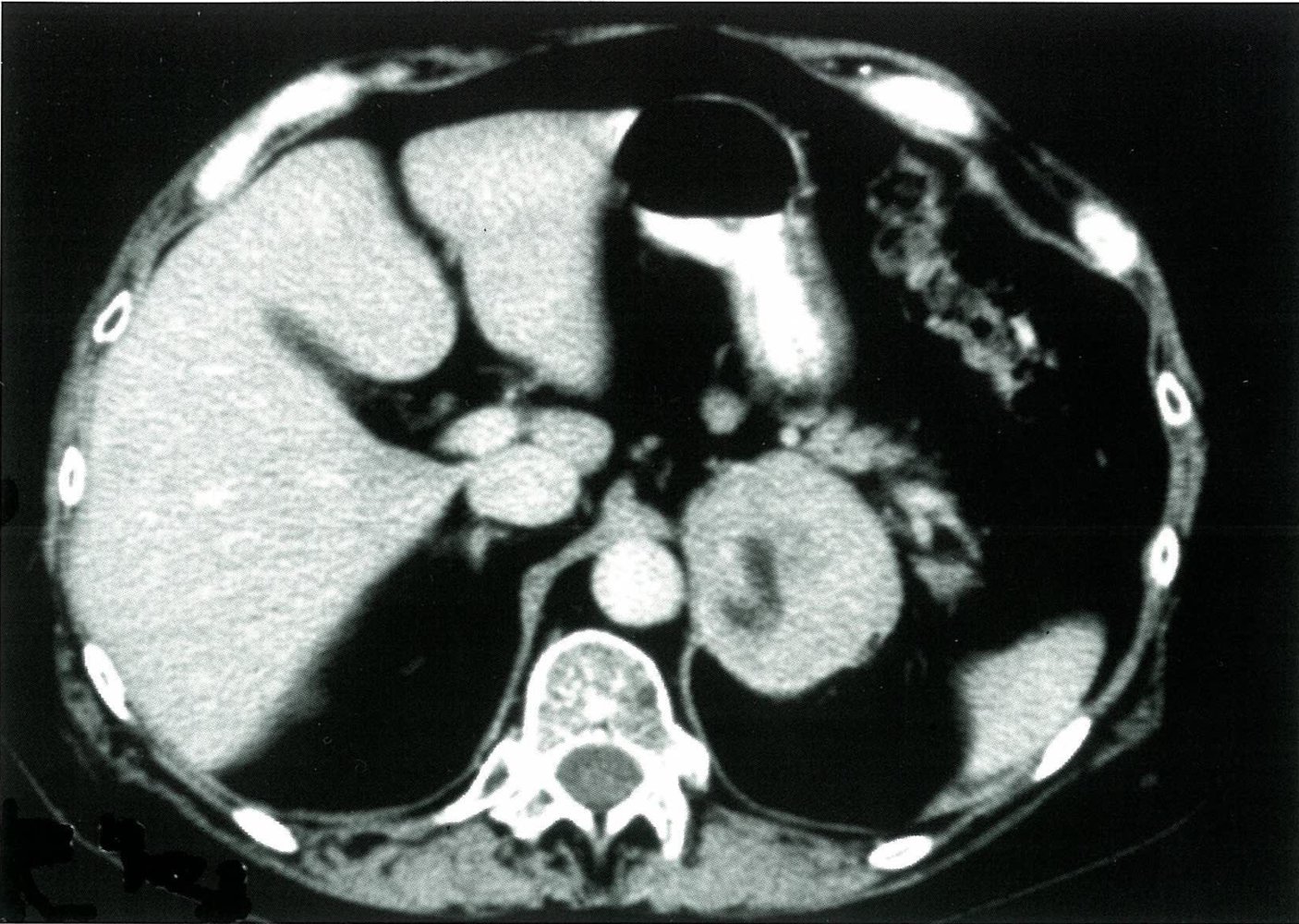
CT without contrast (first-line)[2]
-
Low-risk features for malignancy include:
- ≤ 10 Hounsfield units (HU), i.e., lipid-rich mass
- < 4 cm in diameter [2]
- Homogeneous
-
High-risk features for malignancy include:
- > 10 HU [2]
- ≥ 4 cm in diameter [4]
- Heterogeneity
- Irregular tumor margins, necrosis, vascularity, calcification
-
Interpretation
- Low-risk features: no further imaging required
- Combination of low-risk and high-risk features: Consider additional imaging studies.
- High-risk features : Consider surgery (and/or additional imaging).
A homogeneous adrenal mass with an attenuation (radiodensity) of ≤ 10 HU is considered benign and does not require further imaging.
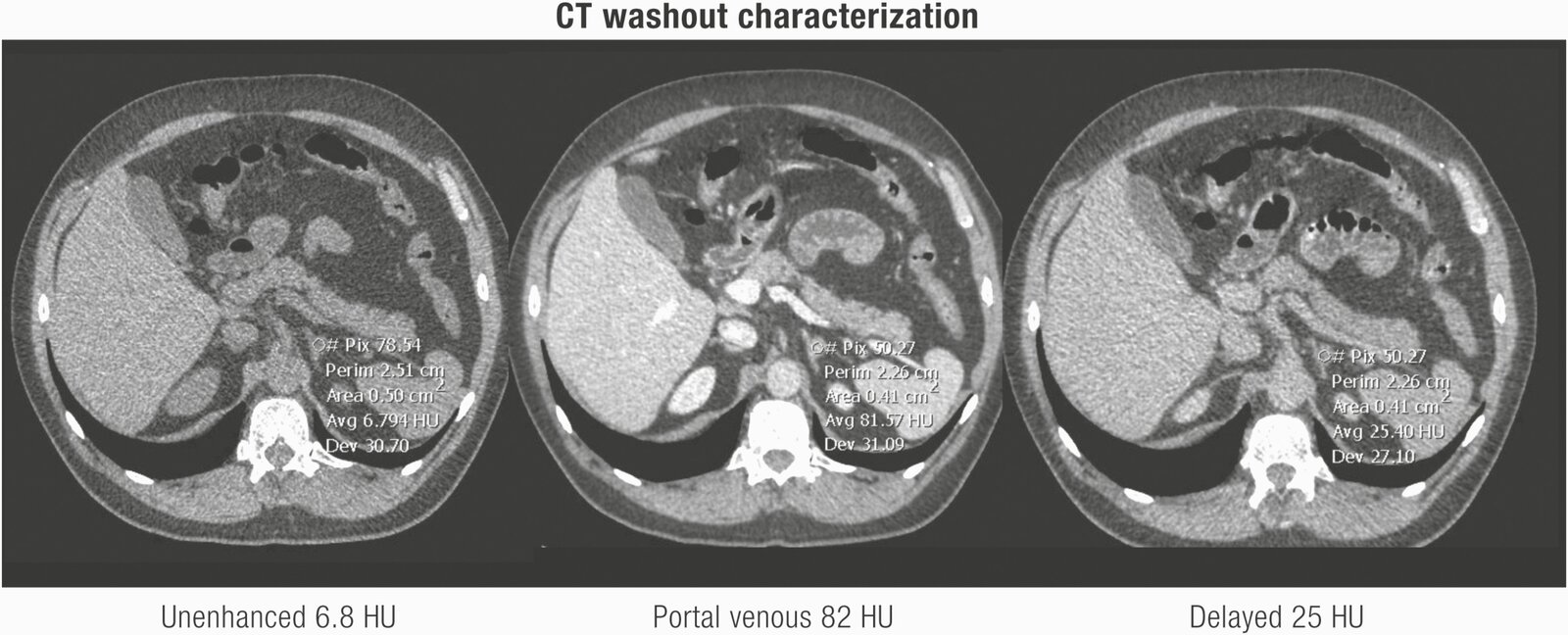
Alternative and additional imaging
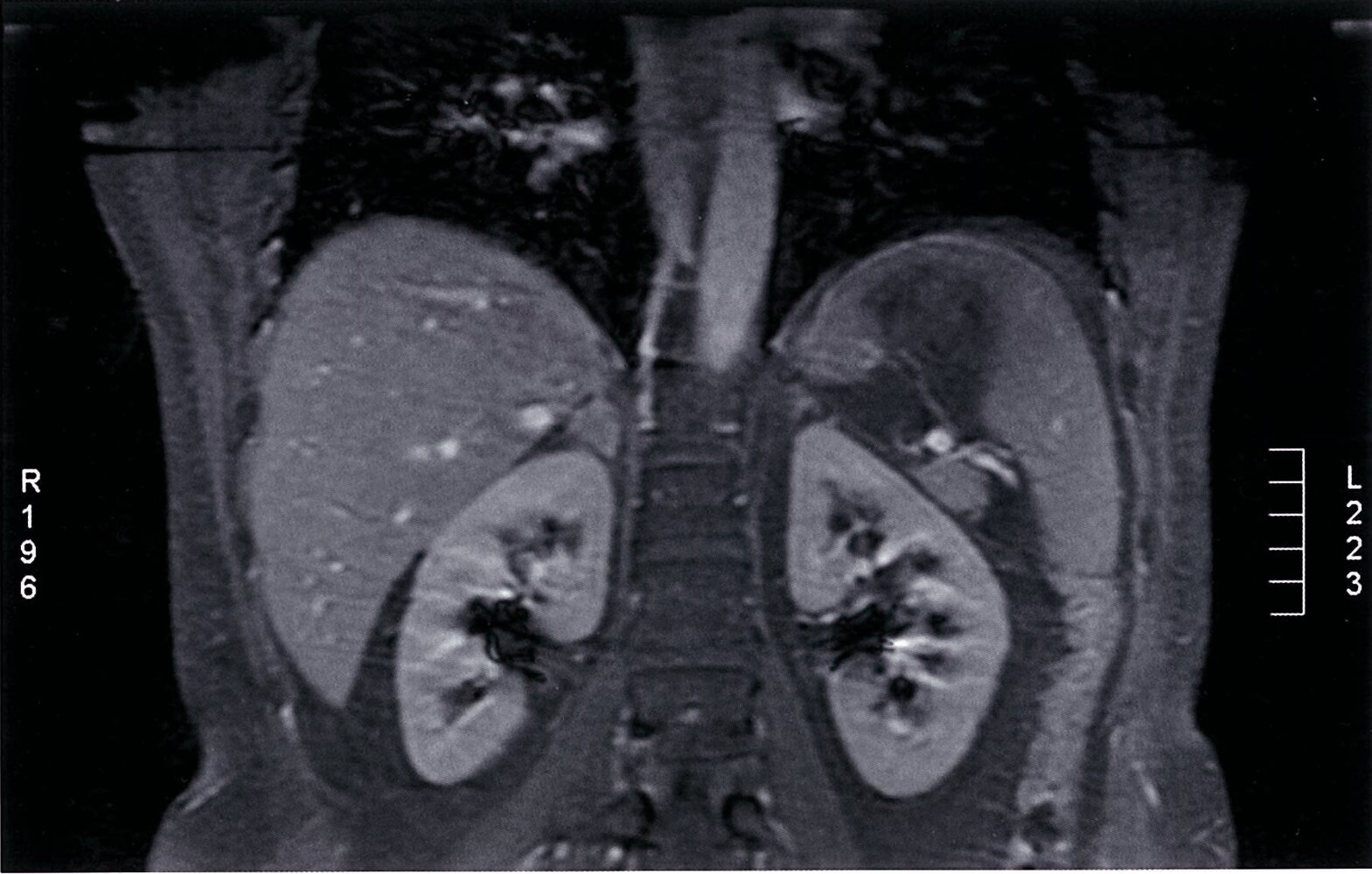
-
MRI with chemical shift analysis
- Alternative to CT to identify benign masses and exclude malignancy
- Offers equivalent information to CT
-
FDG-PET CT
- Mainly used as additional imaging for indeterminate masses on CT/MRI to identify malignancy
- May detect the primary tumor in patients with adrenal metastases
- May detect metastases of a malignant adrenal tumor
- Other: e.g., MRI , CT abdomen (adrenal washout study) [2]
Biochemical testing
The following is an overview of the indications and initial tests for hormonal activity in adrenal incidentaloma. See the respective disease-specific articles for details of confirmatory testing.
| Biochemical testing in adrenal incidentaloma [1][2][4] | |||
|---|---|---|---|
| Endocrine condition | Indication | Initial test | Supportive findings |
| Hypercortisolism |
|
|
|
| Catecholamine excess |
|
|
|
| Hyperaldosteronism |
|
|
|
| Hyperandrogenism, hyperestrogenism, and steroid precursor excess |
|
|
|
| Adrenal insufficiency |
|
|
|
| Congenital adrenal hyperplasia |
|
|
|
Sex hormone-producing adrenal incidentalomas are typically adrenocortical carcinomas.
Histopathology
-
Biopsy [1][2]
- Not routinely recommended
- Indication: suspected adrenal malignancy other than adrenocortical carcinoma if the result is expected to have an impact on management
- Catecholamine excess must be excluded before biopsy.
-
Diagnostic adrenalectomy [2][4]
- Often required for both a definitive diagnosis and treatment in malignant (especially adrenocortical carcinomas) or hormonally active masses
- Additional indication: unclear imaging and/or laboratory findings
Biopsy is rarely indicated in adrenal incidentaloma. However, a definitive diagnosis of adrenocortical carcinoma usually requires adrenalectomy and histopathology.
| Common types of adrenal incidentaloma [1][2][4] | |||
|---|---|---|---|
| Condition | Characteristic clinical features | Diagnostic findings | Management |
| Nonfunctioning adrenocortical adenoma |
|
|
|
| Mild autonomous cortisol secretion |
|
|
|
| Cushing syndrome |
|
|
|
| Primary hyperaldosteronism |
|
|
|
| Pheochromocytoma |
|
|
|
| Adrenocortical carcinoma |
|
|
|
| Metastases |
|
|
|