Introduction
Amaurosis fugax, also known as transient monocular blindness, is a brief episode of vision loss affecting one eye. The most common etiology is a temporary reduction in retinal blood flow due to atherosclerotic emboli from the ipsilateral carotid artery. Although symptoms typically resolve spontaneously in <10 minutes, amaurosis fugax is often a warning sign for future vascular events, such as stroke, making it crucial to recognize and manage promptly.
Pathogenesis
Amaurosis fugax is caused primarily by a transient ischemic attack of the retina, usually due to atherosclerotic emboli originating from the ipsilateral carotid artery. When an embolus occludes an artery supplying the retina (eg, ophthalmic or central retinal artery), hypoxia ensues and results in transient monocular vision deficits. After the embolus is broken up or displaced (spontaneously), retinal perfusion is restored and vision returns, usually within 10 minutes.
Other causes of transient monocular vision loss are less common and include cardioembolic disease, giant cell arteritis, hypercoagulable disorders, retinal vein occlusion, retinal vasospasm, and papilledema.
The temporary nature of the ischemia typically means that no permanent retinal damage occurs, although recurrent episodes can lead to cumulative injury. In addition, patients with amaurosis fugax and concomitant carotid artery disease have an increased risk for future stroke.
Risk factors
The following conditions are associated with an increased risk for amaurosis fugax:
- Carotid artery atherosclerosis
- Hypertension
- Diabetes mellitus
- Hyperlipidemia
- Smoking
- Older age
- Cardioembolic disease (eg, atrial fibrillation, valvular heart disease, endocarditis)
- Giant cell arteritis (a vasculitis most common in patients age 70-80) (Monocular vision loss is typically accompanied by unilateral headache and jaw claudication.)
- Hypercoagulable states (eg, antiphospholipid syndrome, factor V Leiden)
Clinical presentation
Amaurosis fugax characteristically presents with:
- Sudden, painless monocular vision loss:
- Descriptions often reference a "curtain" or "shade" descending over the visual field.
- Vision loss can range from mild blurring to complete blindness and may involve all or part of the visual field (based on the location and extent of retinal ischemia).
- Symptoms typically resolve in <10 minutes, and vision returns to baseline with no residual effects.
- Funduscopic examination, which is often normal, although there may be visible embolic plaques or evidence of underlying chronic disease (eg, diabetic/hypertensive retinopathy)
Differential diagnosis
- Central retinal artery occlusion (CRAO): causes acute-onset, painless monocular vision loss that is prolonged (rather than transient). A cherry-red spot and pale-appearing retina are characteristic findings on funduscopic examination.
- Retinal detachment: can cause significant unilateral vision changes, sometimes described as a "curtain descending" over the eye. However, retinal detachment is most classically preceded by flashes and floaters with vision loss starting in the periphery, and symptoms are unlikely to resolve within minutes.
- Migraine with aura: may be associated with visual changes (eg, scintillating scotoma) or transient visual deficits, but typically presents in younger women with a unilateral throbbing headache, nausea, photophobia, and phonophobia.
- Acute angle-closure glaucoma: is characterized by painful monocular vision loss, headache, and nausea/vomiting. Examination usually shows conjunctival injection with a poorly reactive middilated pupil.
Diagnosis
Amaurosis fugax is mainly a clinical diagnosis based on a history of painless monocular vision loss that resolves spontaneously within minutes, particularly in patients with known atherosclerotic disease or cardiovascular risk factors.
The main focus of the work-up is to identify the etiology of amaurosis fugax and initiate appropriate interventions to prevent future vascular events (eg, CRAO, stroke).
Laboratory evaluation
Laboratory tests typically obtained during the evaluation of amaurosis fugax include:
- Erythrocyte sedimentation rate (ESR) and C-reactive protein assess for giant cell arteritis as the etiology of transient vision loss.
- Blood glucose and lipid profile evaluate for atherosclerotic risk factors.
- Coagulation studies determine whether there is an underlying hypercoagulable disorder.
Imaging studies
The following radiologic tests are usually performed when evaluating amaurosis fugax, particularly in patients age >50 with cardiovascular risk factors:
- Carotid Doppler ultrasonography: to identify carotid artery stenosis or atherosclerotic plaques
- Echocardiography: to detect cardiac embolic sources (eg, valvular vegetation)
- MR angiography or CT angiography: to assess the carotid and intracranial vessels in more detail and rule out alternate diagnoses such as intracranial hemorrhage, mass, or ischemic stroke
ECG is also obtained to evaluate for arrhythmias (eg, atrial fibrillation) that increase the risk of thrombosis/embolism.
Management
Treatment varies based on the underlying condition(s) causing the transient retinal artery occlusion. The goal is to manage cardiovascular risk factors and lower the risk for repeat arterial occlusion.
- Initiate cardiovascular risk management: including blood pressure control, diabetes mellitus management, lipid-lowering medications, smoking cessation, dietary changes, and exercise.
- Consider antithrombotic therapy:
- Antiplatelet therapy: aspirin or clopidogrel to reduce the risk for future ischemic events
- Anticoagulant therapy: in patients with atrial fibrillation or other high-risk disease who are prone to clot formation
- Surgical intervention: includes a carotid endarterectomy ( , which is surgical removal of arterial plaque if carotid stenosis is significant.
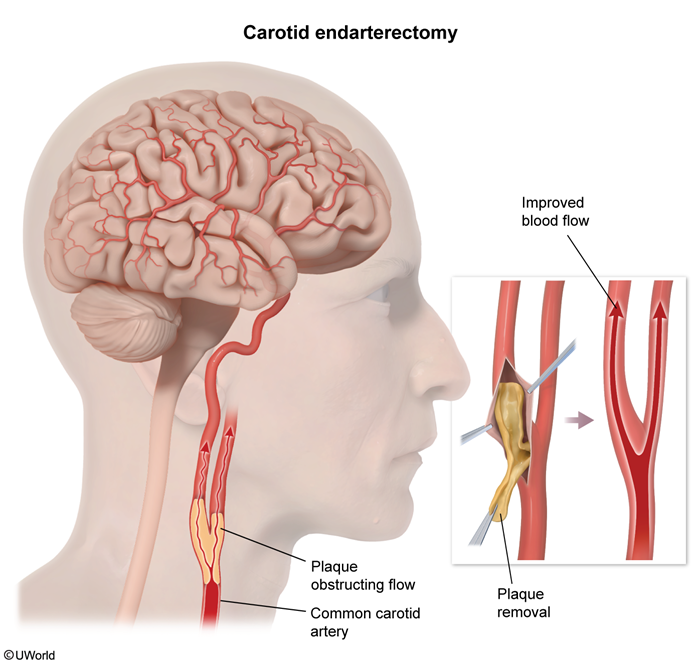 figure 1
figure 1
Prognosis
The prognosis of amaurosis fugax depends on the underlying cause. Although the vision-related outcome is generally good, amaurosis fugax is a warning sign of future cerebrovascular events. Therefore, the risk of stroke or permanent vision loss is significant if the underlying cause is not identified and addressed promptly.
Summary
Amaurosis fugax
characteristically presents with painless, rapid, transient, monocular vision loss. The most common etiology is retinal ischemia due to an embolus originating from carotid artery atherosclerotic plaques. The diagnosis is mainly clinical based on history and the presence of risk factors. Management seeks to reduce cardiovascular risks and prevent future thrombotic/embolic events, particularly because amaurosis fugax with carotid atherosclerosis is associated with an increased risk for stroke.