Amebiasis is an infectious disease caused by the anaerobic protozoan Entamoeba histolytica. Transmission is usually via the fecal-oral route (e.g., through contaminated drinking water) in individuals traveling in an endemic region. Depending on organ involvement, amebiasis is termed either intestinal or extraintestinal. Symptoms of intestinal amebiasis, such as bloody diarrhea and abdominal pain, typically develop after an incubation period of 1–4 weeks. Patients with extraintestinal amebiasis most commonly develop an amebic liver abscess that manifests with right upper quadrant (RUQ) abdominal pain weeks to years after the initial infection. Intestinal amebiasis is diagnosed with stool testing, while extraintestinal amebiasis is typically diagnosed with imaging and serology. Asymptomatic intestinal infection is treated with a luminal cysticidal agent (e.g., paromomycin). Treatment of symptomatic intestinal amebiasis and amebic liver abscesses consists of a nitroimidazole to target invasive trophozoites followed by a luminal cysticidal agent. Image-guided needle aspiration may be indicated for abscesses at risk of perforation or bacterial coinfection.
- E. histolytica is very common in tropical and subtropical regions (e.g., Mexico; , Southeast Asia, India) and affects more than 50 million people worldwide. Amebic infection is relatively rare in the US.
- Men and especially immunocompromised individuals have a higher risk of developing liver abscesses. [1]
Epidemiological data refers to the US, unless otherwise specified.
- Pathogen: : Entamoeba histolytica, a protozoan
-
Transmission
-
Fecal-oral
- Amebic cysts are excreted in stool and can contaminate drinking water or food
- Transmission may also occur through sexual contact.
- Infection typically occurs following travel to endemic regions such as the tropics and subtropics. [2]
-
Fecal-oral

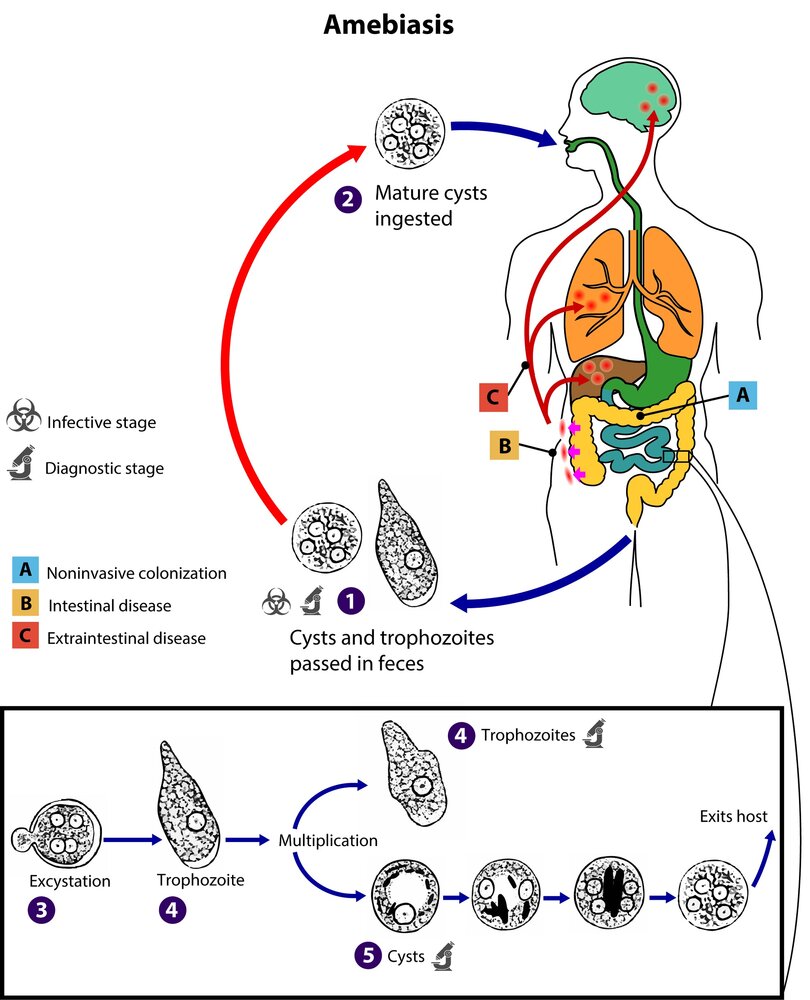
- Life cycle: ingestion of mature cysts → excystation in the small intestine → cysts divide into 4 and then 8 → noninvasive colonization of the colon by trophozoites (may lead to intestinal and extraintestinal disease) → trophozoites encyst → cysts are excreted (along with trophozoites) → cysts are reingested by the same patient or spread to another individual [2]
-
Stages
- Cyst stage: Cysts are very resilient (even against gastric acid) and are able to survive outside the host for months.
- Vegetative stage: trophozoite formation
- Trophozoites can produce proteolytic enzymes that allow them to invade the intestinal submucosa. They can then enter the bloodstream where they consume erythrocytes and disseminate to target tissues like the liver via the portal system.
Definition
- E. histolytica infection confined to the gastrointestinal tract
Clinical features [3][4]
Most infections remain asymptomatic. Only 10–20% of infected individuals develop symptoms. [3]
- Incubation period: : typically 1–4 weeks
- Onset: acute or gradual symptom development
-
Symptoms
- Watery and/or bloody diarrhea
- Abdominal pain, cramps
- Painful defecation, tenesmus
- Weight loss
- Fever (less common)
- Symptoms of fulminant colitis (e.g., hypotension, abdominal distension, peritoneal signs)
Always consider amebiasis when a patient presents with persistent diarrhea after traveling to the tropics or subtropics.
Diagnosis [3][5]
Indications [3][4]
- Symptomatic individuals: abdominal pain, weight loss, bloody and/or watery diarrhea, and recent travel to an endemic area
-
Asymptomatic individuals
- Personal history of endemic exposure (i.e., time spent in an endemic area)
- History of endemic exposure through household members or via sexual contact
Diagnostics [3][5]
-
Stool analysis
- PCR (preferred)
- Antigen detection (e.g., EIA, ELISA)
-
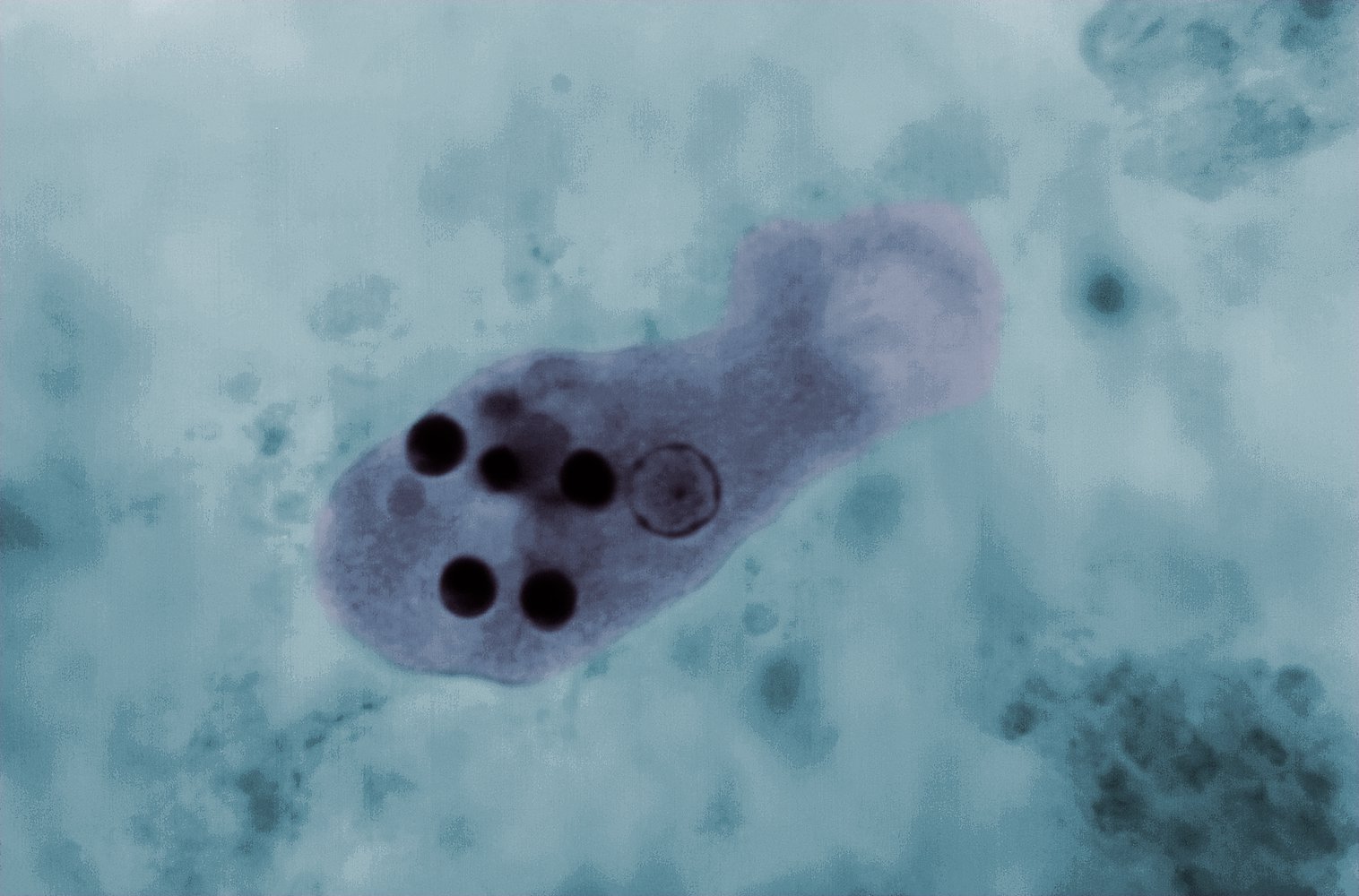
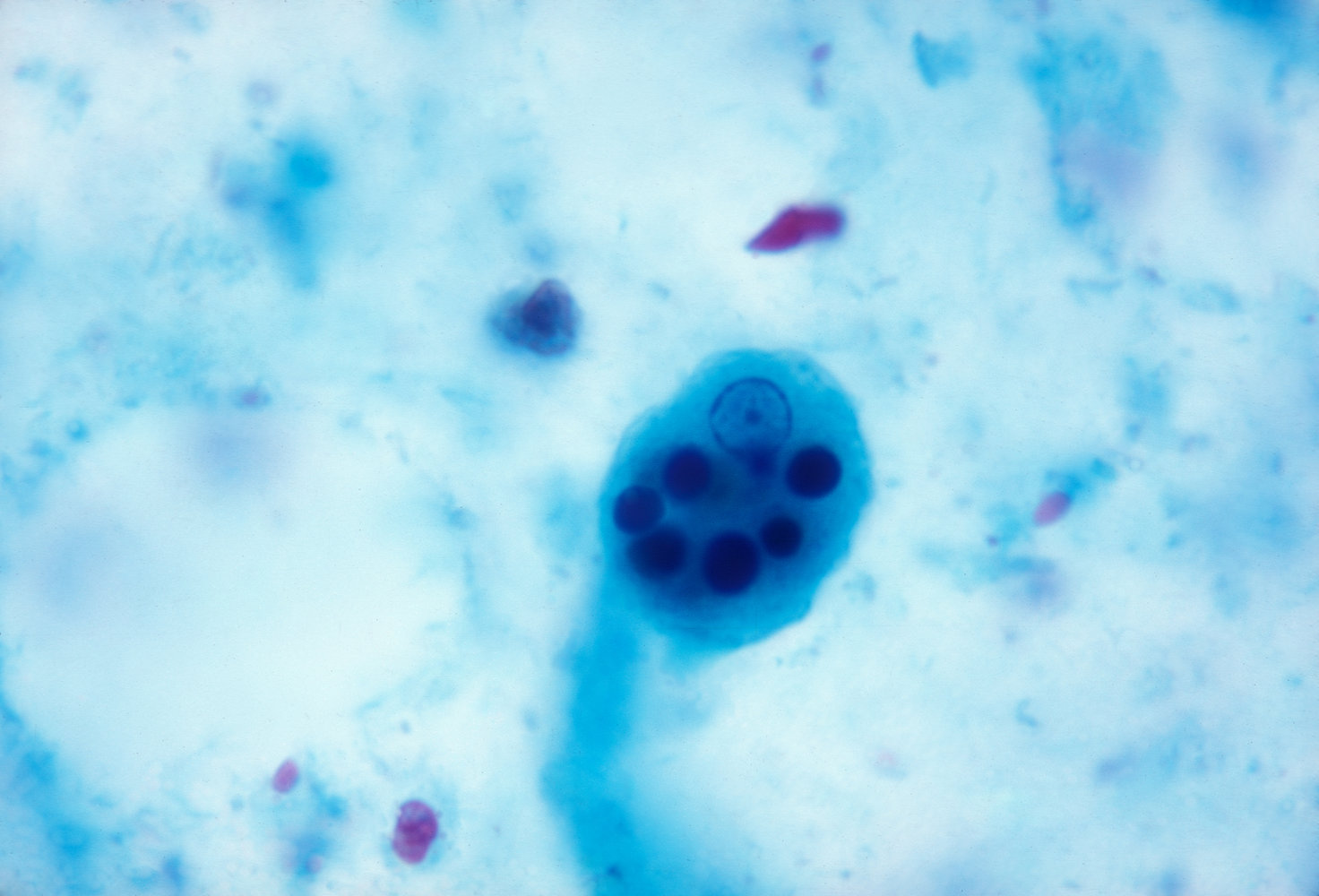
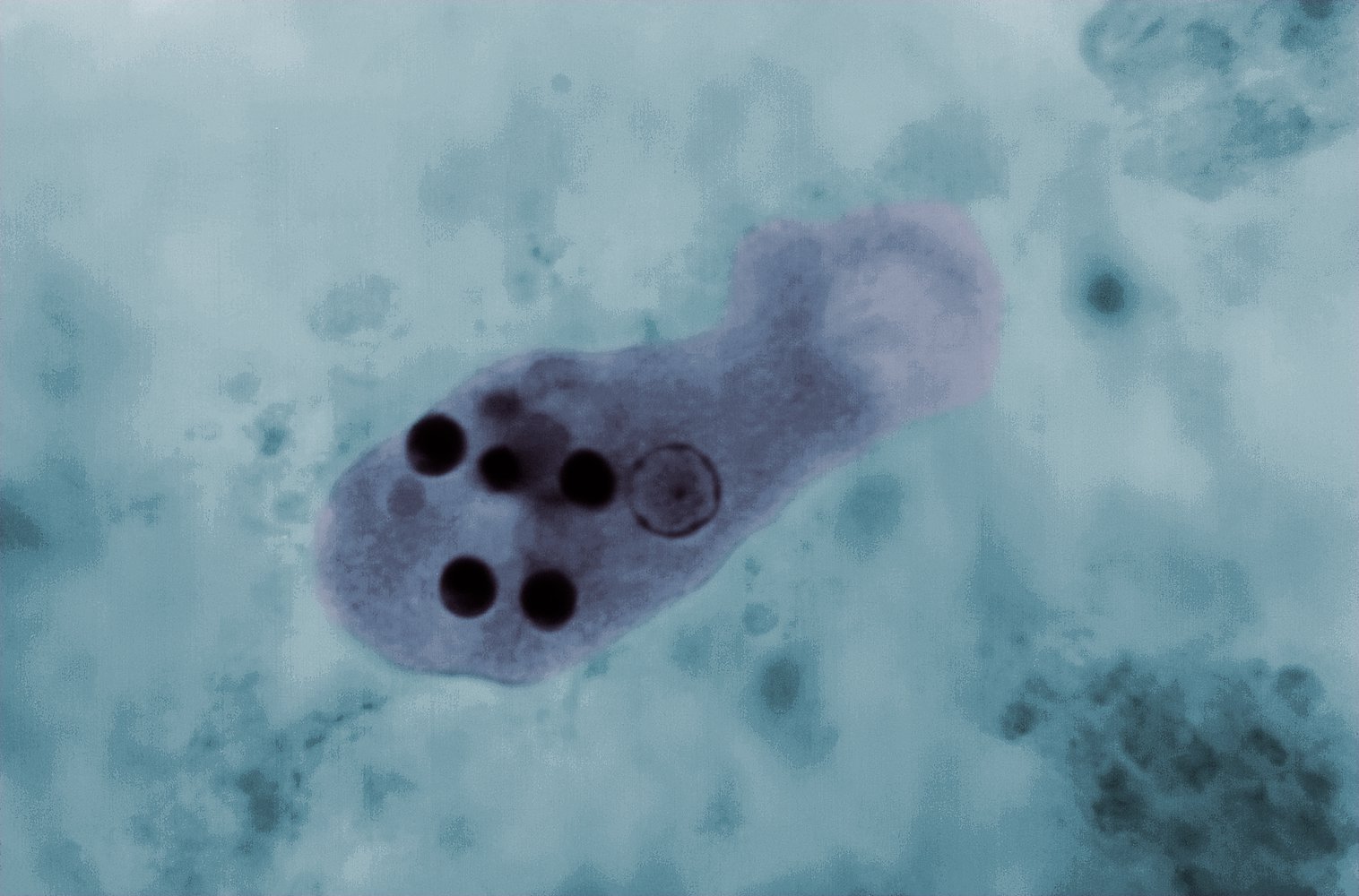
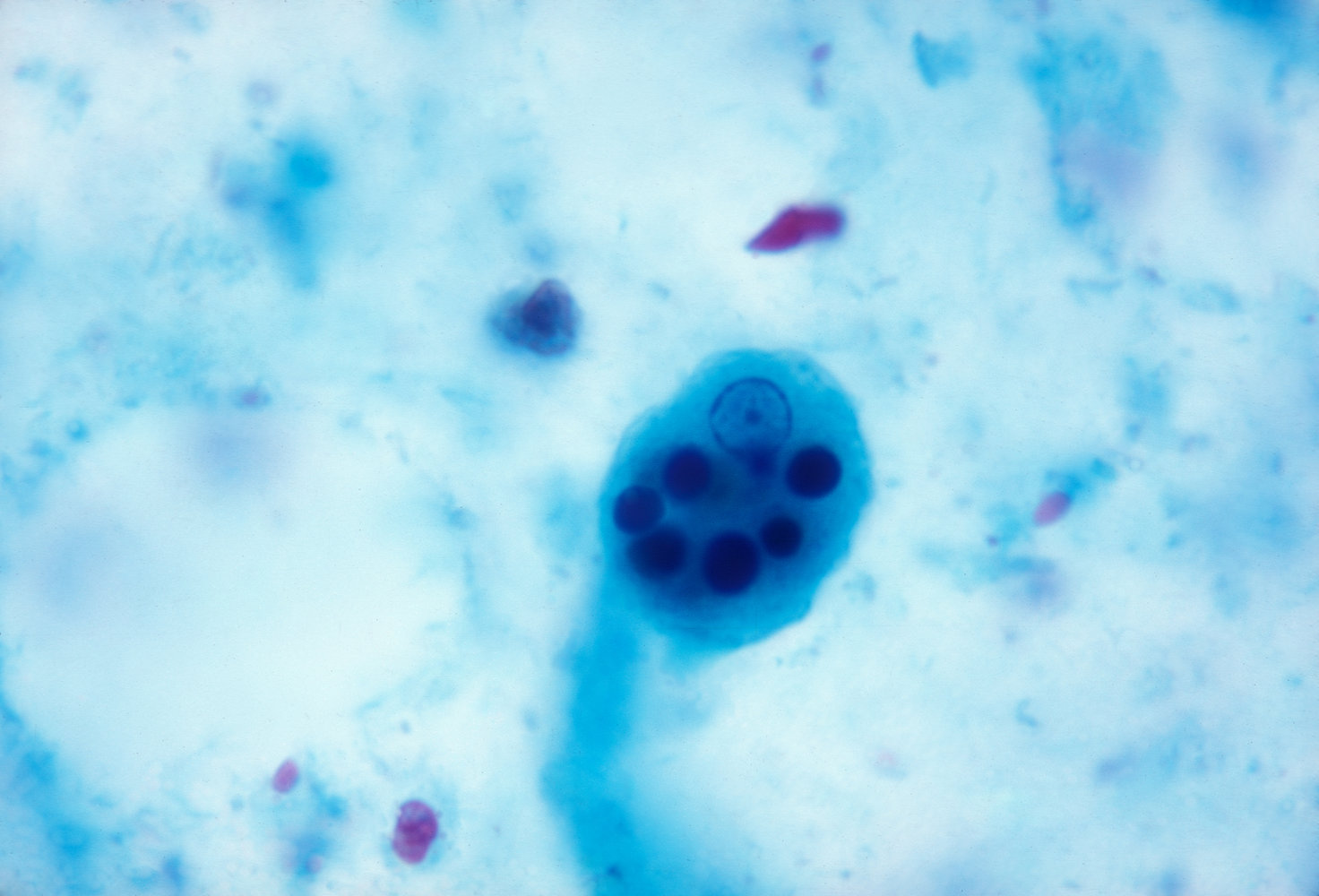
Microscopy: identification of cysts and/or trophozoites in fresh stool ; [3][6]
- Trophozoites often contain ingested erythrocytes.
- Cysts contain up to four nuclei.
- E. histolytica appears morphologically identical to nonpathogenic Entamoeba dispar (E. dispar).
- Serology: detection of antiamebic antibodies in serum [3][5]
- Colonoscopy with biopsy: : flask-shaped ulcers [3][5]
E. histolytica Engulfs Erythrocytes.
Stool microscopy has low sensitivity. Examine ≥ 3 stool samples before reporting a negative result.


Differential diagnosis
- See “Etiology of acute and persistent diarrhea.”
- See “Etiology of chronic diarrhea.”
- See “Viral gastroenteritis.”
- See “Bacterial gastroenteritis.”
- See “Intestinal protozoa.”
- See “Helminths.”
- See “Differential diagnosis of acute abdominal pain.”
Treatment [3][4]
Pharmacotherapy [3][4]
-
Symptomatic individuals: Administer a nitroimidazole to target invasive trophozoitesfollowed by a luminal agent to eradicate intestinal cysts and prevent relapse. ; [3][7]
- Nitroimidazole: metronidazole; for 5–10 daysOR tinidazole for 3–5 days [3]
- Luminal agent: paromomycin; for 7 days (alternatives: diloxanide OR iodoquinol) [3]
-
Asymptomatic individuals: Administer a luminal cysticidal agent to prevent invasive disease and cyst shedding.
- First-line: paromomycin for 7 days [3]
- Alternatives: diloxanide OR iodoquinol
E. dispar is nonpathogenic and does not require treatment. [3]
Management of fulminant amebic colitis [3]
- Consult infectious diseases and general surgery.
- Provide immediate hemodynamic support.
- Consider adding empiric antibiotic therapy for intraabdominal infections.
- Consider surgical intervention for complications (e.g., toxic megacolon, colonic necrosis).
Complications [3]
- Fulminant colitis or necrotizing colitis
- Toxic megacolon leading to colonic perforation
- Ameboma
- Fistula formation (e.g., rectovaginal fistula)
Definition
- E. histolytica infection occurring outside the gastrointestinal tract
- Most commonly manifests as an amebic liver abscess
- Rarely causes abscesses in other organs (e.g., lungs, kidney, brain)
Clinical features [3][4]
- Incubation period: a few weeks to several years [7]
- Onset: usually over 2–4 weeks
-
Symptoms
- Fever (more common)
- RUQ abdominal pain
- Hepatomegaly
- Right-sided pleuritic chest pain and/or referred shoulder pain
- Other GI symptoms: nausea, vomiting, diarrhea, constipation, abdominal distension
- Other organ-specific clinical features rarely occur [4]
Fewer than one third of patients have associated or prior history of diarrhea and/or other gastrointestinal symptoms. [7]
Diagnosis [3][4][7]
- Suspect amebic liver abscess in patients with RUQ abdominal pain, fever, and recent travel to an endemic area.
- Diagnosis is typically based on imaging and confirmed with serologic testing.
Imaging
-
Abdominal imaging: typically shows a solitary lesion in the right lobe of the liver
- Ultrasound (abdomen or liver): round, well-defined, hypoechoic mass
- CT/MRI: round lesion with contrast-enhancing wall
- See also “Diagnosis of intraabdominal abscesses.”
- Additional imaging (e.g., chest, head): Consider if extrahepatic lesions are suspected.
Confirmatory studies
- Serology: detection of antiamebic antibodies in the serum [3][5]
-
Abscess aspiration: not routinely indicated but may be considered to rule out pyogenic liver abscess
- Gross pathology: thick brown pus (resembles anchovy paste)
- Microscopy: acellular debris, trophozoites (in < 20% of patients) [7]
- PCR and/or antigen testing of aspirated material can confirm the diagnosis.
Additional studies
-
Laboratory studies
- CBC: mild to moderate leukocytosis and anemia without eosinophilia
- Liver chemistries: elevated alkaline phosphatase, normal or mildly elevated aminotransferases
- Stool studies (i.e., microscopy, antigen detection, PCR): often negative [3]
Differential diagnosis
- See “Fever.”
- See “Differential diagnosis of acute abdominal pain.”
- See “Intraabdominal abscesses”
- See “Pyogenic liver abscess.”
Treatment [3][4][7]
Manage in consultation with infectious diseases, general surgery, and/or interventional radiology.
-
Pharmacotherapy: a nitroimidazole to target invasive trophozoites followed by a luminal agent to eradicate intestinal cysts and prevent relapse ; [3][7]
- Nitroimidazole: metronidazole; for 10 daysOR tinidazole for 5 days [3]
- Luminal agent: paromomycin; for 7 days (alternatives: diloxanide OR iodoquinol) [3]
-
Indications for imaging-guided percutaneous drainage [3]
- No clinical response to pharmacotherapy within ∼ 72 hours
- High risk of rupture (e.g., abscess size > 5 cm, left lobe abscess)
- Bacterial coinfection (see “Treatment of pyogenic liver abscess”)
- Surgical drainage: typically avoided but may be indicated for amebic liver abscesses that are inaccessible or ruptured with peritonitis
Suspect bacterial coinfection in patients with no clinical response to antiamebic pharmacotherapy within ∼ 72 hours. [4]
Complications
- Pyogenicabscess due to secondary infection [8]
- Peritonitis due to abscess rupture
- Dissemination that may lead to metastatic infection (e.g., brain abscess)
- Direct extension to the pericardium and/or pleura
Food and water hygiene [9]
- Unpeeled fruits or vegetables should not be consumed if there is a potential risk of contamination by Entamoeba histolytica cysts (e.g., endemic region with low hygiene standards).
- Even chlorinated water can contain high concentrations of amebae; therefore, water should be boiled before use.
The main principles of amebiasis prevention concern consumption of potentially contaminated food and water and can be summarized as follows: "Boil it, cook it, peel it, or forget it."