Anticonvulsant drugs are classified as either first-generation (classic) agents or second-generation agents. Second-generation anticonvulsants are usually better tolerated and have a broader therapeutic range than classic anticonvulsant drugs. The choice of drug is guided by the type of seizure. First-line treatment for focal seizures includes, e.g., lamotrigine or levetiracetam, while valproate is used for generalized seizures. While all anticonvulsants have dose-dependent side effects on the central nervous system (e.g., somnolence, nausea), select agents also have other side effects (e.g., gingival hyperplasia caused by phenytoin). Anticonvulsants are also used for pain management (e.g., carbamazepine or gabapentin) and as mood stabilizers in bipolar disorders (valproate).
For more information on the treatment of generalized seizures, see treatment of epileptic seizures.
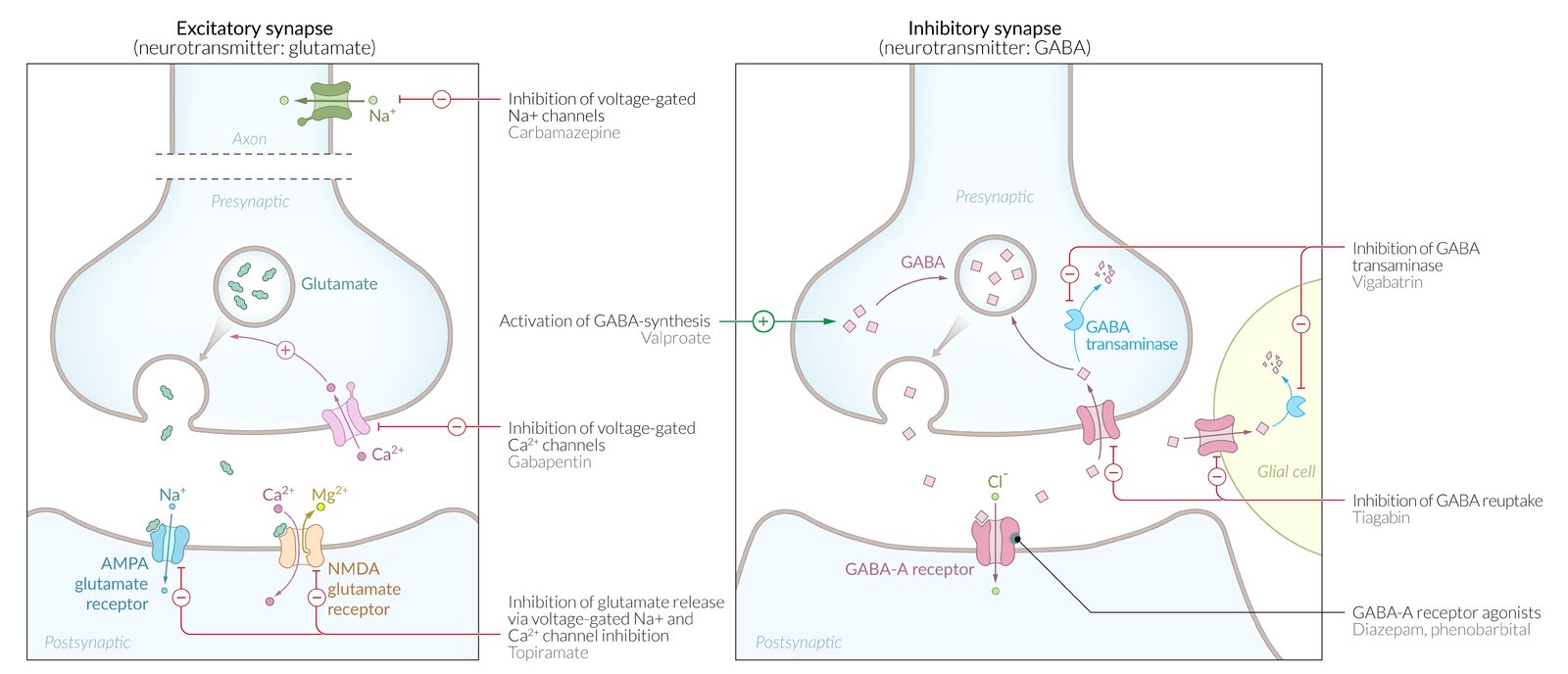
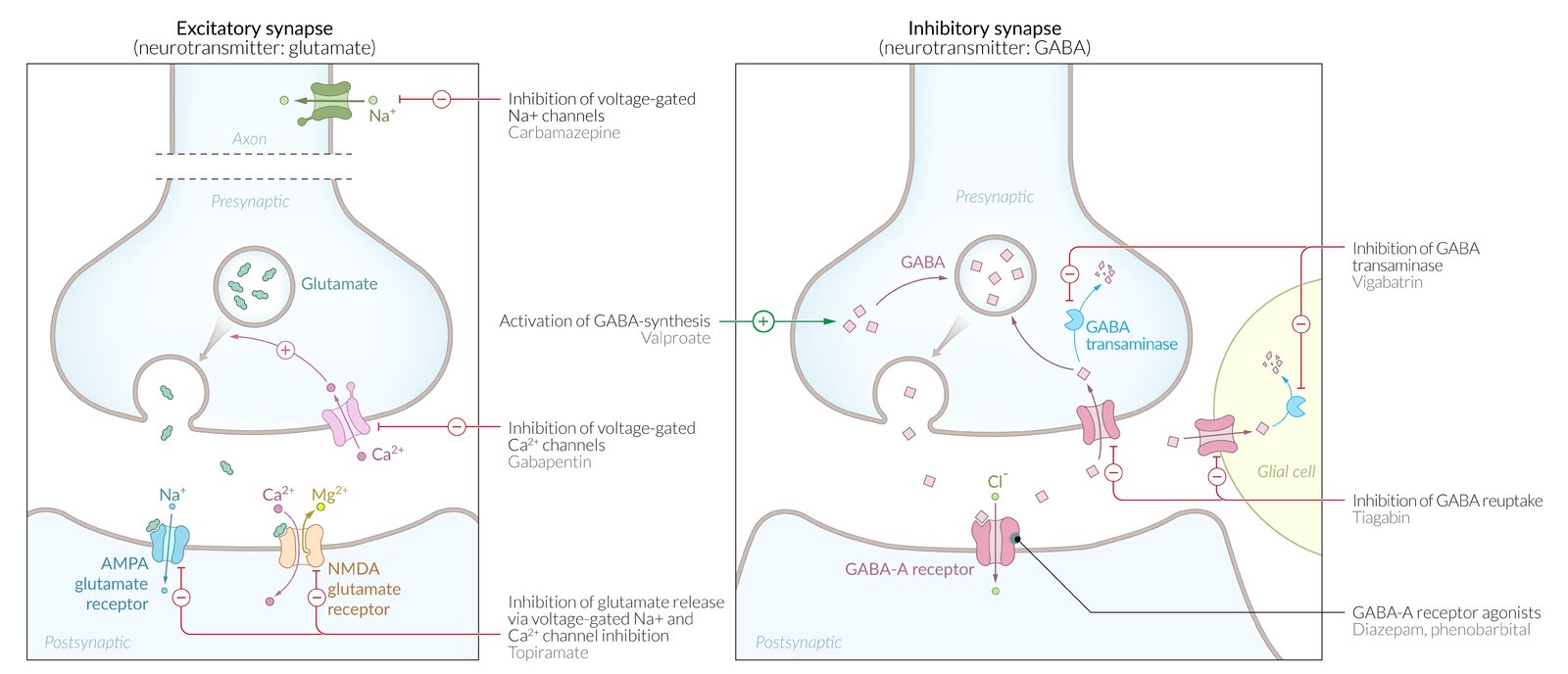
Anticonvulsant drugs inhibit neural activity (↓ neural excitation, ↑ neural inhibition) and increase the seizure threshold by interacting with specific receptors and ion channels.
Overview of first-generation anticonvulsants [1]
| Overview |
|---|
| Agent |
Indication |
Mechanism of action |
Adverse effects |
Contraindications |
Interactions |
| Valproate |
- First-line long-term treatment for tonic-clonic generalized seizures
- Partial (focal) seizures
- Absence epilepsy
-
Treatment of established status epilepticus [2]
- Myoclonic seizures
- Migraine prophylaxis
- Bipolar disorder
|
- Inhibits GABA transaminase → ↑ GABA → ↓ neuronal excitability
- Inactivates Na+ channels and Ca2+ channels
|
- Gastrointestinal upset
- Tremor
- Alopecia
- Pancreatitis
- Weight gain
-
Teratogenicity
-
Especially neural tube defects (contraindicated in women of childbearing age/pregnancy) )
- See pharmacotherapy during pregnancy
-
Hepatotoxicity (usually occurs during the first 6 months of treatment): LFT should be regularly performed in people taking valproate [3]
-
Cytochrome P450 inhibition [4]
- Rash
- Dizziness
- Sedation
- Ataxia
- Thrombocytopenia (may manifest as easy bruising)
- Agranulocytosis
|
- Pregnancy (especially valproate and carbamazepine)
|
- Cytochrome P450 inhibition
|
|
Carbamazepine [5]
|
- First-line treatment for focal seizures
- First-line treatment of trigeminal neuralgia
- Second-line treatment for generalized tonic-clonic seizures
|
|
- Gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea)
- Rash
-
Hyponatremia, hyperhydration, and edema (due to SIADH)
- DRESS syndrome
- Blood count abnormalities (e.g., agranulocytosis, aplastic anemia)
-
Teratogenicity during the first trimester (cleft lip/palate, spina bifida) (see pharmacotherapy during pregnancy)
- Folate depletion
- Diplopia
- Ataxia
- Hepatotoxicity
- Stevens-Johnson syndrome
-
Induces cytochrome P450
- Dizziness
- Sedation
|
- Strong induction of cytochrome P450
|
| Ethosuximide |
-
First-line for absence seizures
|
- Inhibition of voltage-gatedcalcium channels (T-type) in neurons of the thalamus
|
- Gastrointestinal symptoms
- Allergic skin reactions (urticaria, Stevens-Johnson syndrome)
- Pancytopenia
- Fatigue
- Headache
- Myopia
- Sedation
- Dizziness
|
- Increases serum levels of phenytoin
|
| Phenytoin, fosphenytoin |
- Tonic-clonic seizures
- Only rarely used for long-term treatment of focal seizures
-
Treatment of established status epilepticus[2]
|
- Inactivation of Na+ channels
-
Zero-order elimination (i.e., constant rate of drug eliminated)
|
- Hirsutism
-
Hyperpigmentation of skin (melasma)
- Gingival hyperplasia
- Nystagmus
- Osteopenia
-
Megaloblastic anemia due to ↓ folate absorption
- Peripheral neuropathy
- Stevens-Johnson syndrome
- Drug-induced lupus erythematosus
- DRESS syndrome
- Intoxication: sedation, diplopia, ataxia, arrhythmias
- Induction of cytochrome P-450 enzymes
- Teratogenic: fetal hydantoin syndrome
-
Hypothyroidism [6]
- Sedation
- Dizziness
- Rash
- Hepatotoxicity
|
- Induction of cytochrome P450
|
| Phenobarbital |
- First-line treatment in neonates
- Tonic-clonic generalized seizures
- Focal seizures
- Status epilepticus
|
- GABAAagonist → ↑ GABA action
|
- Cardiorespiratory depression
- Tolerance and dependence
- Sedation
- Induces cytochrome P-450
|
| Benzodiazepines |
- First-line for status epilepticus
- Second-line treatment for eclampsia
|
-
Indirect GABAA agonist → ↑ GABA action
|
-
Sedation and dependence (see benzodiazepines)
- Tolerance
- Respiratory depression
|
-
Alcohol, opioids, sedatives: ↑ CNS depression
|
Overview of second-generation anticonvulsants [1]
| Overview |
|---|
| Agent |
Indication |
Mechanism of action |
Adverse effects |
Contraindications |
Interactions |
| Lamotrigine |
- First-line treatment for long-term therapy of focal seizures
-
Second-line treatment for generalized seizures and absence seizures
-
Mood stabilizer for treatment of bipolar disorder
|
- Inhibition of voltage-gated Na+channels → ↓ glutamate release
|
-
Rash, exfoliative dermatitis, or rarely, Stevens-Johnson syndrome (slow titration is necessary to prevent skin and mucous membrane reactions)
- Hemophagocytic lymphohistiocytosis
- Rarely hepatotoxic or nephrotoxic
- Blurry vision
-
Gastrointestinal symptoms
- Sedation
- Dizziness
- DRESS Syndrome
|
|
- Coadministration of carbamazepine, phenobarbital, phenytoin → ↑ clearance
|
| Tiagabine |
-
Focal seizures, with or without impairment of consciousness (adjunctive therapy)
|
- Inhibits GABA reuptake → ↑ GABA
|
- Dizziness
-
Gastrointestinal upset: nausea, vomiting, diarrhea
- Insomnia
- Drowsiness
- Weight changes
|
| Levetiracetam |
- First-line treatment for long-term therapy of focal seizures
- Generalized seizures
|
- Not fully understood
- Blockage of SV2A receptor → GABA and/or glutamate release modulation and inhibition of voltage-gated Ca2+ channels
|
- Lethargy, fatigue
- Nausea
- Headache
- Psychiatric symptoms (e.g., personality changes)
- Sedation
- Dizziness
|
- No significant interactions
|
| Gabapentinoids |
Pregabalin (tentative FDA approval) |
- Drug combination for long-term treatment of focal seizures
- Neuropathic pain
- Neuralgia after herpes infection
- Generalized anxiety disorder
|
-
Inhibition of presynaptic P/Q-type Ca2+ channels via action on the α2δ-subunit → ↓ Ca2+ intracellular flow → ↓ glutamate release [1]
- Does not bind to GABA receptors despite being a GABA analog
|
- Somnolence
- Nausea
- Ataxia
- Impaired vision
- Weight gain
|
| Gabapentin |
-
Second-line treatment for focal seizures
- Postherpetic neuralgia
- Peripheral (poly)neuropathy
|
- Dry mouth
-
Somnolence, nausea
- Ataxia
- Dizziness
- Weight gain
|
-
Morphine: ↑ concentrations of gabapentin
|
| Vigabatrin |
- Refractory focal seizures (adjunctive therapy)
- Monotherapy for infantile spasms (West syndrome)
|
- Inhibits GABA transaminase irreversibly → ↑ GABA
|
|
|
- Decreases serum levels of phenytoin
|
| Topiramate |
- Focal and generalized tonic-clonic epileptic seizures
- Migraine prophylaxis
- Idiopathic intracranial hypertension
|
-
Blockage of voltage-gated Na+
channels
- ↑ GABA
|
- Angle-closure glaucoma
- Weight loss
- Kidney stones
-
Cognitive dysfunction (e.g., decreased verbal fluency, cognitive speed, and working memory)
- Sedation
- Dizziness
- Mood disturbance, depression
- Paresthesia
|
- Decreases efficacy of oral contraceptives
|
You can use the following to remember the features of PHENYTOIN: cytochrome P-450 interaction, Hirsutism, Enlarged gums (gingival hyperplasia), Nystagmus, Yellow-browning of skin (melasma), Teratogenicity, Osteomalacia, Interacts with folate, Neuropathy
To remember that the most important side effects of ethoSUXimide are Steven-Johnson syndrome, fatigue, headache, ABdominal upset, and ALLErGies (e.g., urticaria), think of “It sucks that Steven's FATher has given everyone a headache with his ABsurd ALLEGorizations.”
To remember a crucial side effect of vigabatrin, think of “Vision goes away by accident.”
To remember that phenobarbital is first-line treatment for neonates, think of “Phenobarbital is phenomenal for treating babies.”
To remember that the most common side effects of topiramate are speech impairment, weight loss (light), cognitive impairment, sedation, and kidney stones, think of “It leaves you speechless how lightly the cog railway travels through sediments and stones to the top.”
References:[1][7]
- Monotherapy should always be the first-line treatment: increase the dosage of the drug to the therapeutic range before initiating combination therapy
- Combination therapy: drugs from different classes and/or with different pharmacologic modes of action for refractory seizures [8]
- For more detailed approaches to seizure treatment and epilepsy, see treatment of epileptic seizures.
References:[7][8]
Pregnancy and breastfeeding
- Classic anticonvulsants (especially carbamazepine and sodium valproate!) should be avoided if possible → teratogenic effects
- Newer anticonvulsants: lack of medical data and trials during pregnancy [9]
- The choice of treatment depends on the type of seizure and which substance enables optimal control of seizures.
-
Approach
- Optimize seizure control prior to conception.
- Avoid multiple therapies.
- Administer the drug at the lowest dose that controls seizures.
- Monitor plasma drug levels regularly.