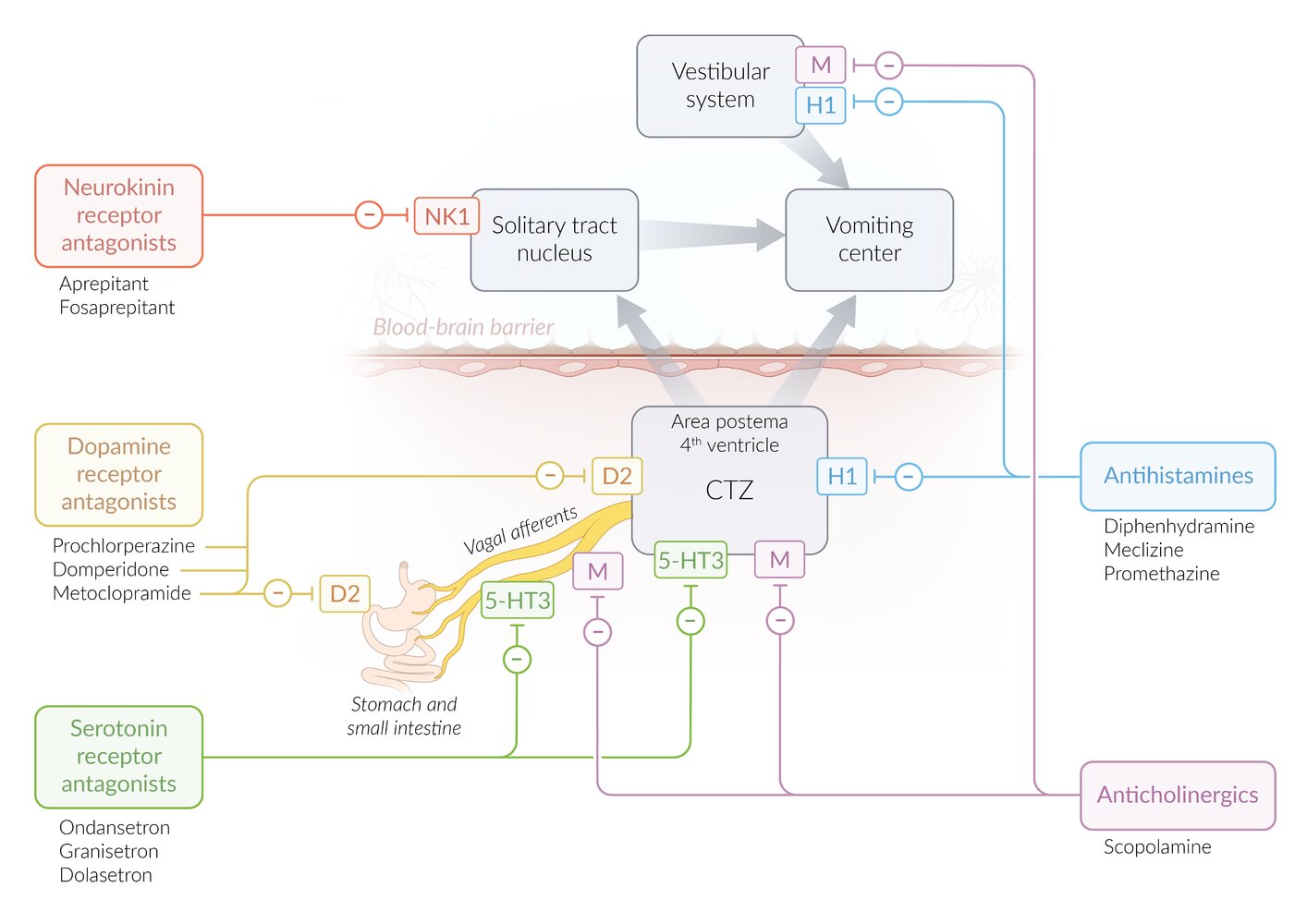
Antiemetics are a heterogeneous group of drugs used to treat various causes of nausea and vomiting. Different antiemetics act on different receptors, and they may have a peripheral effect, a central effect, or both. Whereas serotonin antagonists, for example, bind 5-HT3 receptors and effectively combat cytotoxic drug nausea, certain anticholinergic drugs target M1 receptors and specifically treat motion sickness (kinetosis). Hospitals and clinics commonly use the dopamine D2 antagonist metoclopramide. However, because of its strong central effect and possible extrapyramidal side effects, metoclopramide must be used with caution.
Antiemetics in adults
| Overview of antiemetics in adults | ||||
|---|---|---|---|---|
| Antiemetic class | Drug | Mechanism of action | Clinical use | Side effects |
| Dopamine receptor antagonists |
|
|
|
|
|
|
|
||
|
|
|
|
|
| Serotonin receptor antagonists (5-HT3 antagonists) |
|
|
|
|
| Anticholinergic agents [4] |
|
|
|
|
| Antihistamines |
|
|
|
|
| Neurokinin receptor antagonists |
|
|
|
|
| Glucocorticoids |
|
|
|
|
| Benzodiazepines [8][9] |
|
|
|
|
| Atypical antipsychotics [8][9][10][11] |
|
|
|
|
| Cannabinoids [8][12][13] |
|
|
|
|
Antiemetics in children [14]
-
Ondansetron is commonly used for nausea and vomiting in children, e.g.:
- Acute gastroenteritis with dehydration in ER settings: PO ondansetron (off-label) [15][16][17]
- GI emergencies
- IV ondansetron (off-label) [16]
- PO ondansetron (off-label) [16]
- Chemotherapy-induced nausea and vomiting (CINV): The dosage and route vary by indication; consult a specialist.
- Postoperative nausea and vomiting prevention: ondansetron
- Alternative agents may be used for specific indications; consult a specialist.
- Motion sickness or vertigo: e.g., diphenhydramine (off-label) , dimenhydrinate [18]
- Migraine: e.g., prochlorperazine, metoclopramide [19]
- CINV: e.g., dexamethasone, neurokinin receptor antagonist [20]
- Nonspecific nausea and vomiting
- Chemotherapy-induced nausea and vomiting
- Vertigo (e.g., vestibular neuritis, Ménière's disease)
- Motion sickness
- Gastrointestinal motility disorder (e.g., due to diabetic gastroparesis)
- Postoperative nausea and vomiting
References:[21]
-
Dopamine receptor antagonists
- Intestinal obstruction (ileus)
- Prolactin-dependent tumors
- Parkinson disease: unlike domperidone, metoclopramide and prochlorperazine can cross the blood-brain barrier and exacerbate the pre-existing dopamine deficiency that causes parkinsonism.
- Serotonin receptor antagonists: : severe liver disease, prolonged QT interval
-
Anticholinergic agents and antihistamines
- Tachyarrhythmias, heart failure
- Urinary retention, BPH
- Glaucoma
- Pyloric stenosis
References:[21]
We list the most important contraindications. The selection is not exhaustive.