Antifungals are a class of medications that destroy or inhibit the growth of fungal organisms and are, accordingly, used to treat fungal infections (mycoses) such as candidiasis, cryptococcal disease, aspergillosis, and dermatophytosis. They are divided into three major groups according to chemical structure and spectrum of efficacy: polyenes (used for the treatment of systemic fungal infections), azoles (broad-spectrum antifungals), and allylamines (used for the treatment of onychomycosis). Topical agents (e.g., clotrimazole) generally have a more limited scope of action. Common adverse effects include hepatotoxicity, skin reactions, headaches, and gastrointestinal upset.
See also “Overview of fungal infections,” “Management of superficial fungal infections,” and “Management of systemic fungal infections.”
| Overview of antifungals and their mechanisms of action [1][2][3][4][5][6][7] | ||||||
|---|---|---|---|---|---|---|
| Class | Examples | Mechanism of action | Clinical use | Adverse effects | ||
| Polyenes |
|
|
|
|
||
|
|
|
||||
| Azoles | Triazoles |
|
|
|
|
|
|
|
|||||
|
|
|||||
|
|
|||||
| Imidazoles |
|
|
||||
|
|
|||||
| Allylamines |
|
|
|
|
||
| Echinocandins |
|
|
|
|
||
| Pyridone derivatives |
|
|
|
|
||
| Benzofurans |
|
|
|
|
||
| Antimetabolites |
|
|
|
|
||
-
Overview
- Used mainly for the treatment of systemic fungal infections
- Considered a subgroup of macrolide antibiotics [8]
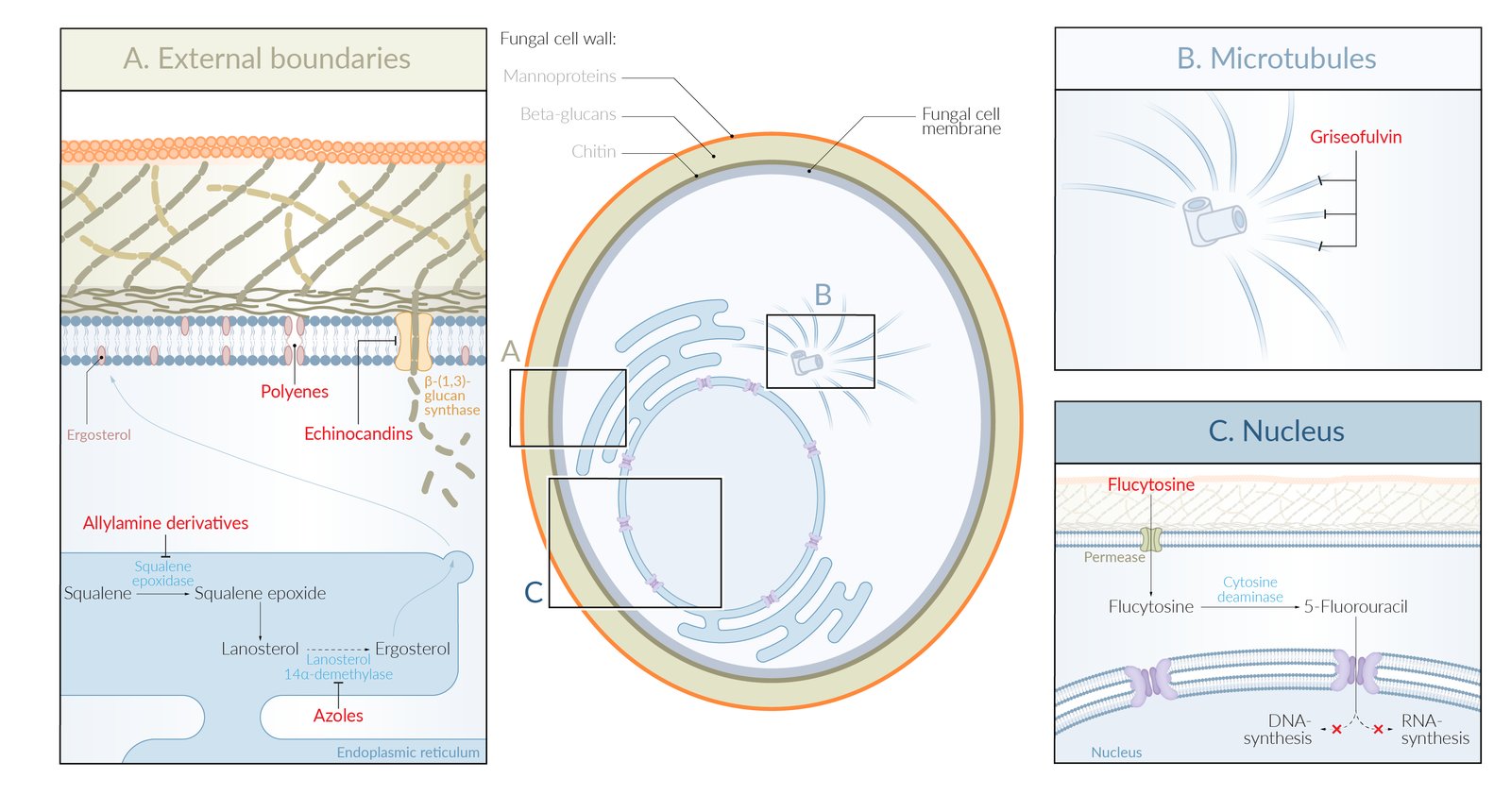
- Mechanism of action: bind to ergosterol in the fungal cell membrane → formation of pores in the fungal membrane → disruption of electrolyte balance → cell lysis → cell death
Amphotericin B Burrows nice (nystatin) holes in the fungal cell membrane.
-
Routes of administration
- Intravenous
- Intrathecal
- Bladder irrigation
-
Clinical use [9]
-
Severe systemic mycoses, such as:
- Cryptococcal disease (in combination with flucytosine for cryptococcal meningitis)
- Sporotrichosis
- Aspergillosis
- Blastomycosis
- Candidiasis
- Coccidioides (administered intrathecally for coccidioidal meningitis)
- Histoplasmosis
- Mucormycosis
- Fungal cystitis
- Fungal meningitis
-
Severe systemic mycoses, such as:
-
Adverse effects [9]
- Nephrotoxicity: Lipid-based formulations of the drug and IV hydration reduce nephrotoxicity.
- IV phlebitis
- Impaired renal tubule permeability → hypokalemia and hypomagnesemia (restoring K+ and Mg2+ while administering the drug can counter this effect)
- Fever, chills; (amphotericin B is sometimes referred to as “shake and bake”)
- Bone marrow suppression, anemia
- Arrhythmias
- Hypotension
-
Contraindications [9]
- Electrolyte disturbances (e.g., hypokalemia, hypomagnesemia)
- Renal dysfunction
- Pregnancy
Amphotericin B has amphoterrible side effects, including nephrotoxicity, arrhythmias, and IV phlebitis.
-
Routes of administration (too toxic for intravenous use)
- Topical: diaper rash
- Oral (swish and swallow): oropharyngeal candidiasis
-
Adverse effects
- Gastrointestinal symptoms (e.g., diarrhea, nausea, pain)
- Contact dermatitis
- Stevens-Johnson syndrome
- Contraindications: pregnancy
Nystatin is too toxic for intravenous use. For oropharyngeal candidiasis, the medication should be swished around in the mouth, gargled, and then swallowed (swish and swallow).
- Definition: a group of antifungal agents with a broad spectrum of activity that can be divided into triazoles and imidazoles
-
Routes of administration
- Imidazoles: topical, oral
- Triazoles: oral, IV
-
Mechanism of action
- Inhibition of 14-alpha demethylase, a fungal cytochrome P450 → ↓ fungal synthesis of ergosterol from lanosterol → ↓ levels of ergosterol → membrane instability → cellular death. [10]
- Ketoconazole: inhibition of 17α-hydroxylase/17,20-lyase
| Overview of azoles | ||||
|---|---|---|---|---|
| Active substance | Clinical use | Adverse effects | ||
| Topical use | Systemic use | |||
| Imidazole derivatives |
|
|
|
|
| ||||
|
|
|||
| Triazole derivatives |
|
|
||
|
|
|||
|
|
|||
|
|
|||
|
|
|||
-
Contraindications
- Cardiac arrhythmias
- Severe cardiac insufficiency
-
Special considerations
- Inhibition of cytochrome P450 can influence serum concentrations of other medications
- Cautious use in patients with renal and/or hepatic dysfunction
- PPIs must be discontinued (azoles require a low pH to be absorbed)
Voriconazole is the drug of choice for inVasive aspergillosis.
The FLU easily penetrates the blood-brain barrier: FLuconazole has good CNS penetration.
- Route of administration: oral
- Mechanism of action: inhibition fungal squalene epoxidase → ↓ synthesis of ergosterol → accumulation of squalene → ↑ membrane permeability → cell death
-
Clinical use
- Dermatophytosis (most commonly onychomycosis)
- Tinea infections (e.g., tinea pedis)
-
Adverse effects
- Hepatotoxicity
- Dysgeusia
- Gastrointestinal upset
- Headache
- Exacerbation of autoimmune diseases (e.g., systemic lupus erythematosus)
-
Contraindications
- Impaired liver function
- Systemic lupus erythematosus
- Breastfeeding
-
Drugs
- Caspofungin
- Anidulafungin
- Micafungin
- Route of administration: IV
- Mechanism of action: inhibition of β-glucan synthesis → disruption of fungal cell wall synthesis →↓ resistance against osmotic forces →cell death
-
Clinical use
- Invasive aspergillosis
- Invasive candidiasis (particularly biofilm-embeddedCandida)
-
Adverse effects
- Flushing (due to release of histamine)
- Hepatotoxicity
- Gastrointestinal upset
- Hypotension
- Phlebitis/pain at the injection site
- Fever, shivering
- Route of administration: topical
-
Mechanism of action
- Not fully understood
- Likely disruption of DNA, RNA, and protein synthesis
-
Clinical use
- Pityriasis versicolor
- Dermatophytosis (e.g., onychomycosis)
- Seborrheic dermatitis of the scalp
-
Adverse effects
- Facial edema
- Ventricular tachycardia
- Skin irritations
- Pruritus
- Route of administration: oral
- Mechanism of action: griseofulvin binds to keratin precursor cells → accumulation in keratin-rich tissues (e.g., nails, hair) → entry into the fungal cell → interference with microtubule function → disruption of fungal mitosis
- Clinical use: dermatophyte infections (e.g., tinea pedis)
-
Adverse effects
- Hepatotoxicity
- Carcinogenicity
- Teratogenicity
- Enzyme induction → ↓ concentration of many drugs metabolized by cytochrome P450 (e.g., warfarin)
- Confusion, headaches
-
Disulfiram-like reaction
- A reaction similar to the disulfiram-ethanol reaction triggered by the concomitant intake of alcohol and another drug (e.g., griseofulvin, procarbazine, some cephalosporins)
- Clinical signs of a disulfiram-like reaction include flushing, tachycardia, and hypotension.
- Urticaria and severe skin reactions (e.g., Stevens-Johnson syndrome)
-
Contraindications
- Porphyria
- Hepatic failure
- Pregnancy and breastfeeding
- Route of administration: oral
- Mechanism of action: converted to 5-fluorouracil by fungal cytosine deaminase, thereby inhibiting DNA and RNA synthesis
-
Clinical use
- Combination with amphotericin B: systemic fungal infections (especially cryptococcal meningitis)
- Monotherapy: non-life-threatening infections, such as genitourinary candida infections, that do not respond to other drugs
-
Adverse effects
-
Bone marrow suppression with pancytopenia
Hepatic injury - Renal failure
- Gastrointestinal upset
-
Bone marrow suppression with pancytopenia
-
Contraindications
- Renal impairment
- Pregnancy and breastfeeding
See also “Treatment of superficial fungal infections” and “Treatment of systemic fungal infections.”
| Treatment of common fungal infections | |||
|---|---|---|---|
| Treatment | |||
| Candidiasis | Mucocutaneous | Oropharyngeal |
|
| Esophageal |
|
||
| Vaginal |
|
||
| Cutaneous |
|
||
| Invasive |
|
||
| Invasive aspergillosis |
|
||
| Cryptococcosis |
|
||
| Blastomycosis Histoplasmosis Coccidioidomycosis Sporotrichosis |
|
||
| Pityriasis versicolor |
|
||
| Dermatophytosis |
|
||