Antithyroid drugs are drugs that either decrease thyroid hormone synthesis (thionamides) or thyroid hormone release (iodides). The most important group of antithyroid drugs are thionamides, which include methimazole, carbimazole, and propylthiouracil. Thionamides decrease thyroid hormone synthesis by inhibiting thyroid peroxidase, an essential enzyme involved in multiple steps of thyroid hormone synthesis. Thionamides play a significant role in the treatment of hyperthyroidism and thyroid storm. Iodides are solutions containing potassium iodide that inhibit the release of thyroid hormones into the circulation. They are, therefore, a useful adjunct treatment in the management of thyroid storm, but their main clinical use is for the preoperative preparation of a patient with Graves' disease, because they decrease the vascularity of the thyroid gland.
| Overview of antithyroid drugs | ||
|---|---|---|
| Thionamides | Potassium iodides | |
| Examples |
|
|
| Mechanism of action |
|
|
| Onset |
|
|
| Indications |
|
|
| Special considerations |
|
|
References:[1][2][3]
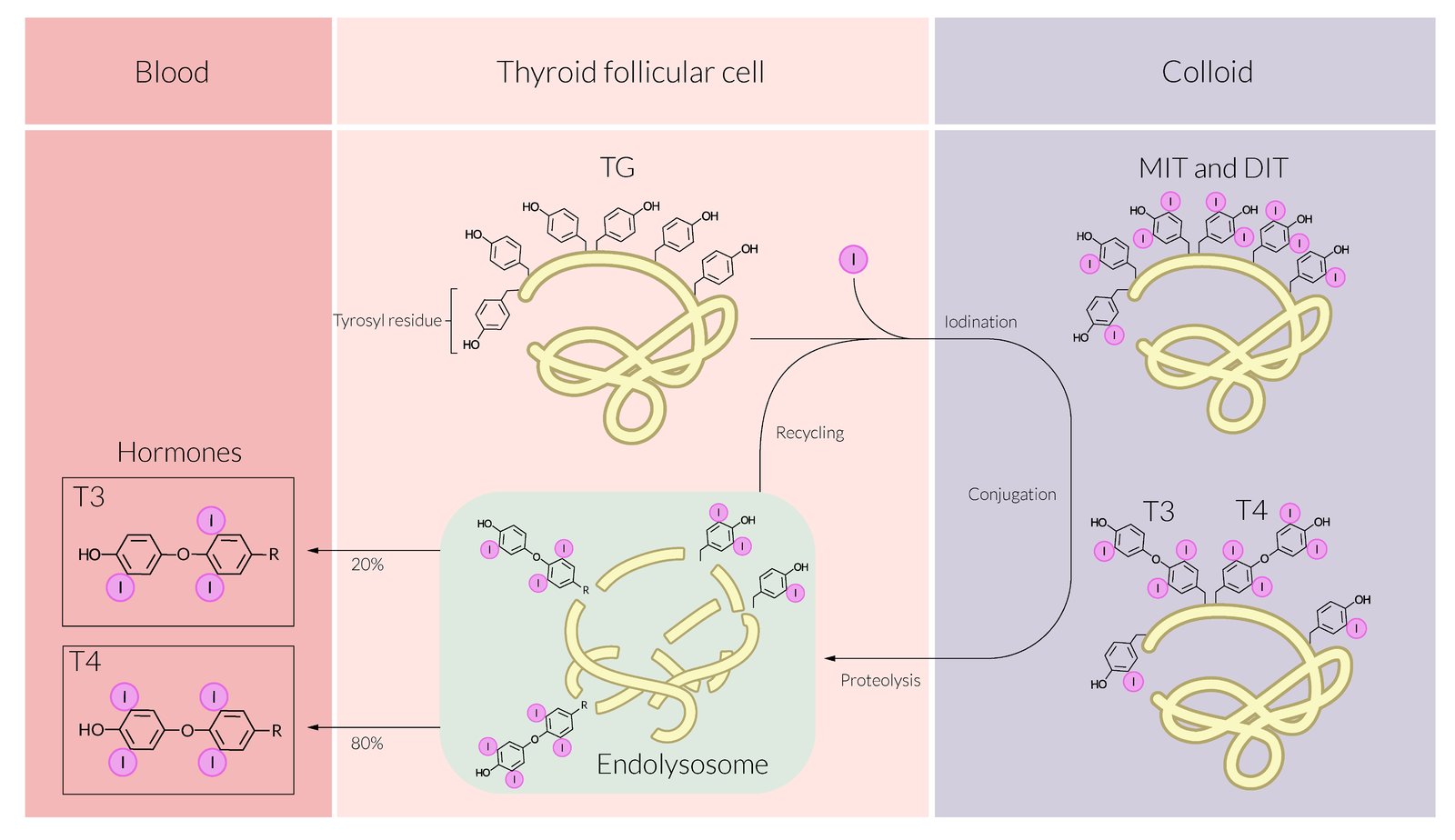
See thyroid hormone synthesis.
Thionamides
-
Allergy/hypersensitivity
- The most common side effect is a pruritic rash (particularly with methimazole)
- Rarely, severe effects such as exfoliative dermatitis, ANCA-associated vasculitis (propylthiouracil), polyserositis, and acute arthralgia occur
- If mild, switch to propylthiouracil; if severe, avoid thioamides because of the risk of cross-sensitivities
-
Hematologic side effects
-
Agranulocytosis
- Rare but dangerous (affects ∼ 0.5% of patients; more common in elderly and those taking high doses)
- Rapidly reversible with discontinuation of treatment
- Aplastic anemia
- Thrombocytopenia
-
Agranulocytosis
-
Hepatotoxicity (seen with propylthiouracil use)
- Hepatitis
- Cholestatic jaundice
- Liver failure
- Teratogenicity: increased risk of congenital malformations with carbimazole and methimazole (e.g., aplasia cutis)
-
Other
- Diffuse goiter
- Impaired sense of taste (dysgeusia)
As methimazole and carbimazole are teratogenic, propylthiouracil is recommended in the first trimester. After the first trimester, switch back to carbimazole or methimazole because of the hepatotoxic effects of propylthiouracil.
Iodides
- Side-effects are rare and often mild.
- Oral/gastric mucosal irritation (e.g., aphthous ulcers, metallic taste): To avoid mucosal irritation, iodides should be consumed with food or diluted with fluids.
- Allergy/hypersensitivity: rash, angioedema; rarely, severe anaphylactic reactions can occur
- Teratogenicity: contraindicated in pregnancy because they can cross the placental barrier and cause fetal goiter
- Iodides delay and decrease the effects of radioactive iodine. They must be stopped at least a week before radioactive iodine ablation.
References:[2][3][4]
We list the most important adverse effects. The selection is not exhaustive.