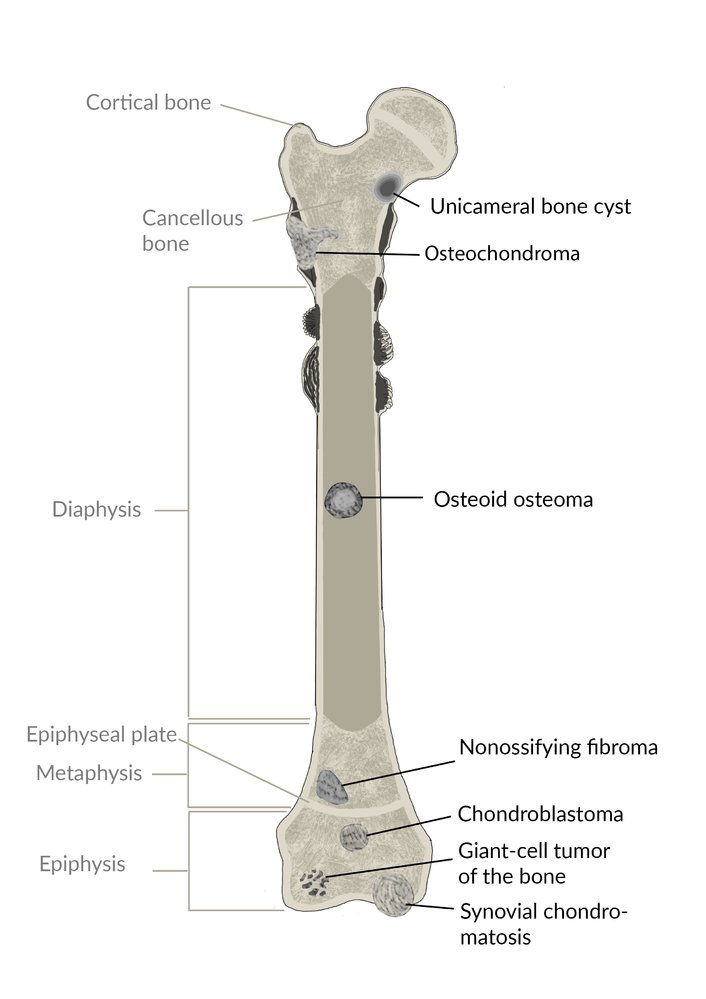
Benign bone lesions are a heterogeneous group of slow-growing neoplasms that arise from cartilage or bone. They appear on x-ray as localized lesions with sharp margins and without soft tissue involvement. Surgical removal or curettage may be required to manage pain and/or prevent pathological fractures.
Benign bone tumors are usually asymptomatic and do not require treatment until they become symptomatic (pain, swelling, etc).Surgery is indicated for symptomatic lesions and may involve curettage, bone grafting, or resection.
Predominantly osseous tumors
| Overview of predominantly osseous tumors | ||||
|---|---|---|---|---|
| Type | Description | Epidemiology | Location | Characteristics |
| Osteoid osteoma |
|
|
|
|
| Osteoblastoma |
|
|
|
|
| Giant-cell tumor (osteoclastoma) |
|
|
|
|
| Osteoma |
|
|
|
|
| Torus palatinus |
|
|
|
|


Tumors with cartilaginous components
| Overview of tumors with cartilaginous components | ||||
|---|---|---|---|---|
| Description | Epidemiology | Location | Characteristics | |
| (Distal) enchondroma |
|
|
|
|
| Chondroblastoma |
|
|
|
|
| Synovial chondromatosis |
|
|
|
|
| Osteochondroma (cartilaginous exostosis) |
|
|
|
|
Fibrous lesions
| Overview of fibromas | ||||
|---|---|---|---|---|
| Description | Epidemiology | Location | Characteristics | |
| Nonossifying fibroma |
|
|
|
|
| Ossifying fibroma |
|
|
|
|
| Fibrous dysplasia |
|
|
|
|
Cysts and hemangiomas
| Overview cysts and hemangiomas | ||||
|---|---|---|---|---|
| Type | Description | Epidemiology | Location | Characteristics |
| Unicameral bone cyst |
|
|
|
|
| Aneurysmal bone cyst |
|
|
|
|
| Intraosseous hemangioma |
|
|
|
|
| Langerhans cell histiocytosis |
|
|
|
|
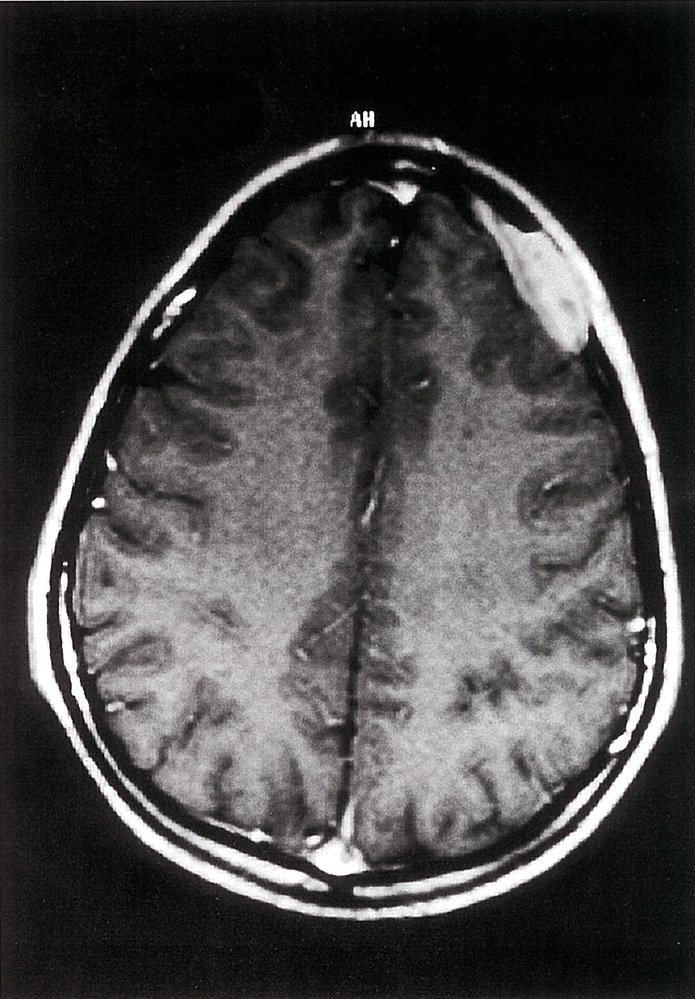
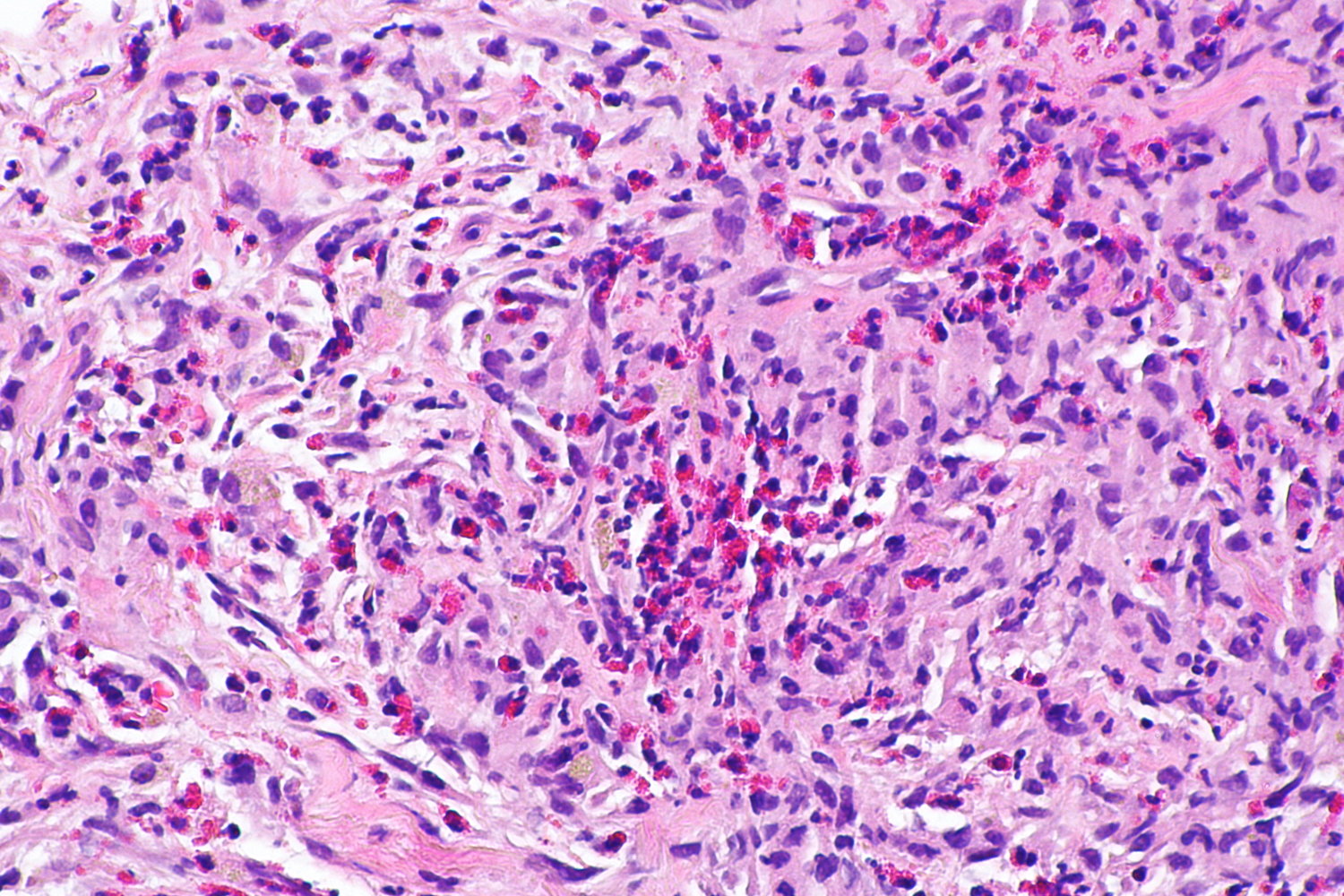
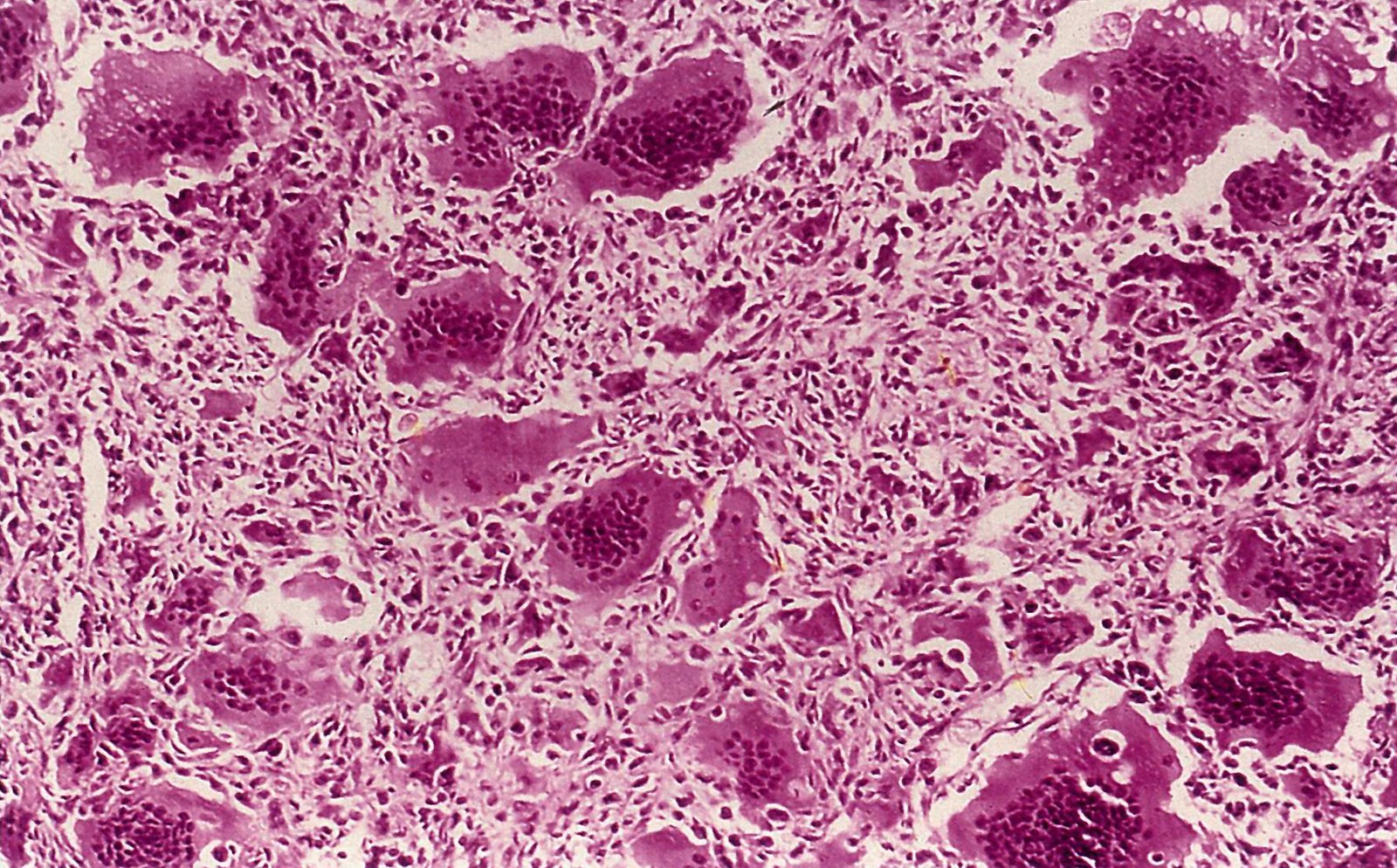
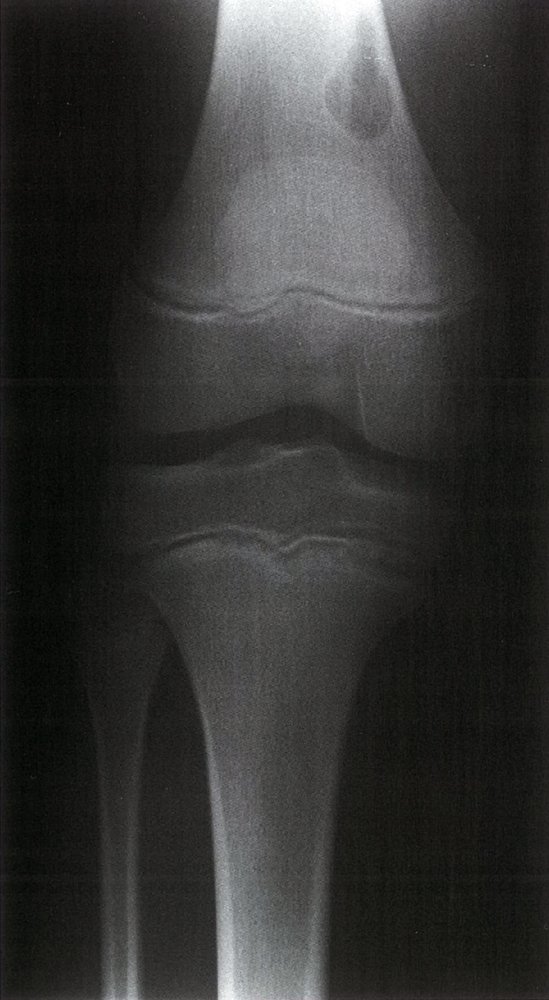
- Description: benign but locally aggressive tumor composed of giant cells that arise from the bone marrow [1]
- Epidemiology: peak incidence between 20 and 40 years
-
Clinical features
- Found in the epiphysis or metaphysis of long bones (especially knee region)
- Pathological fractures
- Local pain and swelling
- Limited range of motion
-
Diagnostics
- X-ray: multicystic osteolytic lesions (soap-bubble appearance)
-
Histopathology
- Mononuclear, RANKL-expressing cells (neoplastic)
- Multinucleated giant cells (are reactive and resemble osteoclasts)
- Treatment: curettage and bone grafting or en-bloc resection to minimize recurrence rate
- Prognosis: risk of malignant degeneration increases with age; may spread to the lungs

-
Description
- Bony outgrowth (exostosis) with a cartilaginous cap on the surface of long bones adjacent to growth plates
- Contains a marrow space that is continuous with the underlying bone
-
Epidemiology
- Most common primary benign bone tumor
- Peak incidence: 10–30 years [2]
- Sex: ♂ > ♀
-
Clinical features
- Typically located in metaphysis of long bones
- Usually asymptomatic, but can be painful and palpable near the ends of long bones
-
Subtypes and variants: hereditary multiple exostoses (EXT)
- Definition: autosomal dominant disorder with multiple exostoses
- Most commonly caused by autosomal dominant inheritance of a germline mutation in the EXT tumor suppressor gene.
- Malignant degeneration to chondrosarcoma may occur (∼ 5% of cases).
- Diagnostics: x-ray shows pedunculated; or sessile; lesion on the surface of the metaphysis of long bones
- Treatment: excision of tumor in symptomatic cases
- Complications: Approx. 1% transform into chondrosarcoma.



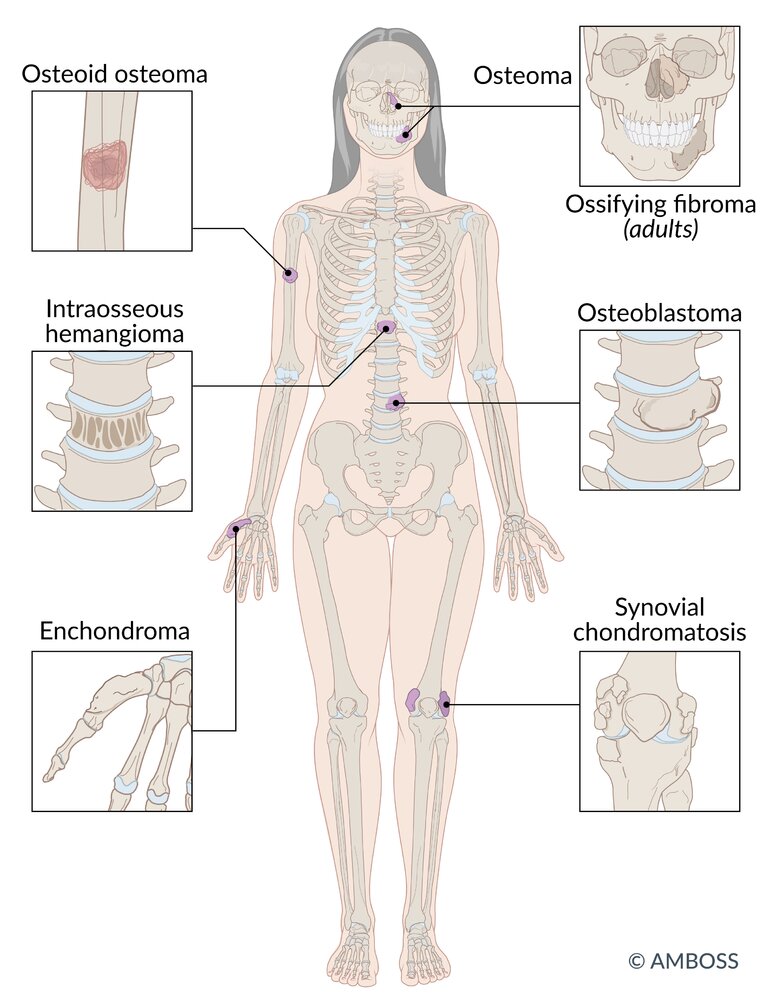
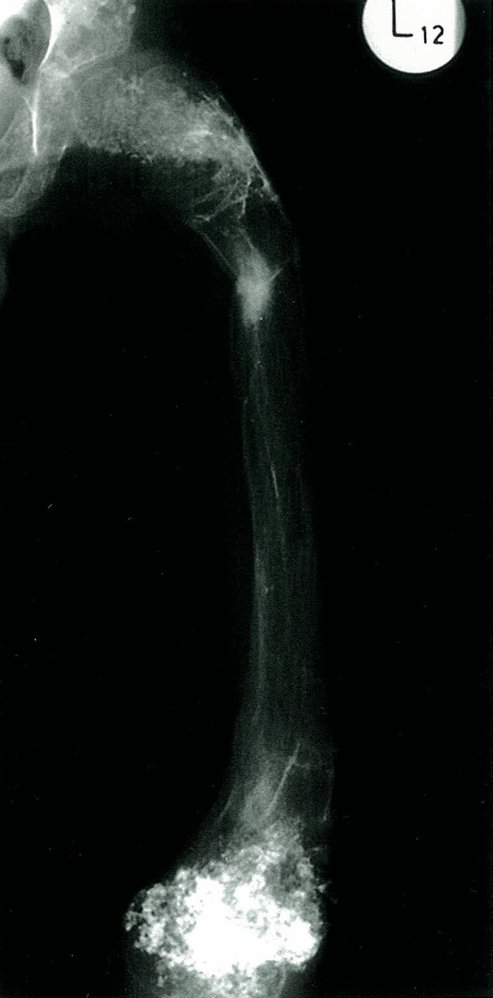
- Description: benign tumor arising from hyaline cartilage
-
Epidemiology
- Most common type of hand tumor
- Peak incidence: 20–50 years (but may occur at any age)
-
Clinical features
- Usually found in medulla of the long bones of the hands and feet (most often the metacarpals of the hand and phalanges of the fingers)
- Often painless
- Widening of the bone
- Pathological (spontaneous) fractures
-
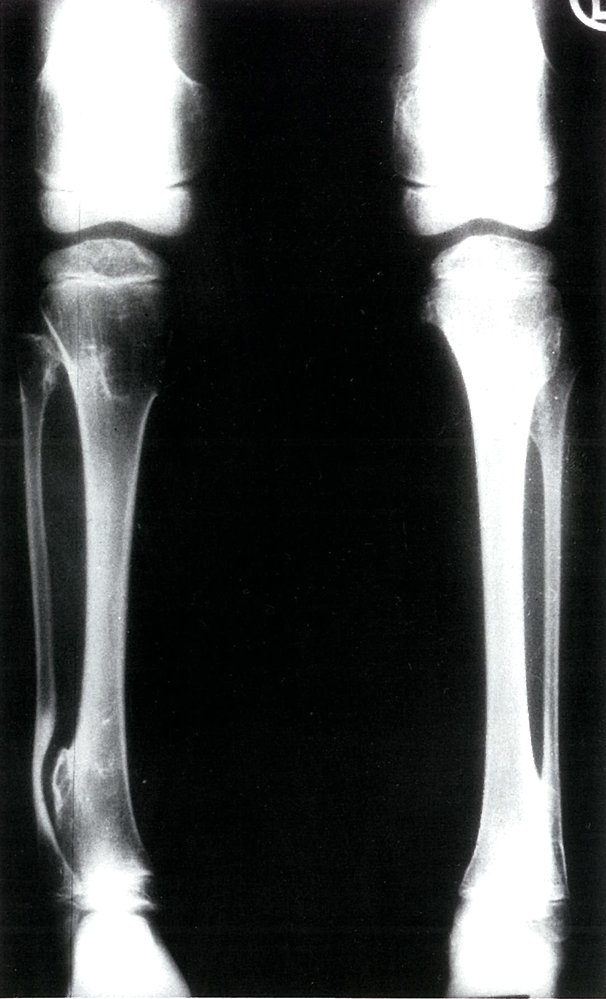
Subtypes and variants: enchondromatosis [3]
- Definition: A predominantly hereditary condition that manifests with multiple enchondromas.
- Epidemiology: peak incidence between 10 and 20 years
- Clinical features: often leads to skeletal deformities and stunted growth
- Prognosis: increased risk of malignant degeneration to chondrosarcoma
-
Treatment
- Asymptomatic tumors do not require treatment and close monitoring suffices.
- Symptomatic tumors may require surgical curettage and subsequent bone grafting to prevent pathological fractures.

- Description: benign cartilage tumor
-
Epidemiology
- Very rare
- Peak incidence: 10–20 years
-
Clinical features
- Located in epiphysis of long bones
- Joint pain (constant) and swelling
- Treatment: surgical curettage and bone grafting
- Description: cartilage formation as a result of metaplasia of the synovial tissue
- Epidemiology: peak incidence between 20 and 40 years
-
Clinical features
- Most commonly located in the knees
- Pain, effusion, reduced range of motion, knee locking
- Diagnostics: x-ray shows radiographically visible (calcified) loose bodies
- Treatment: removal of loose bodies and synovial tissue
- Prognosis: extremely low risk of malignant degeneration to synovial chondrosarcoma

Osteoid osteoma [4]
-
Description
- Small tumor (< 2 cm)
- Predominantly located in the cortex of long bones
-
Epidemiology
- Peak incidence: 4–25 years [5]
- Sex: ♂ > ♀
-
Clinical features
- Located in metaphysis and diaphysis of long bones (predominantly the proximalfemur, tibia, and humerus) and vertebrae
- Constant, intense pain that worsens at night
- Pain is responsive to NSAIDs (e.g., ibuprofen, aspirin)
-
Diagnostics
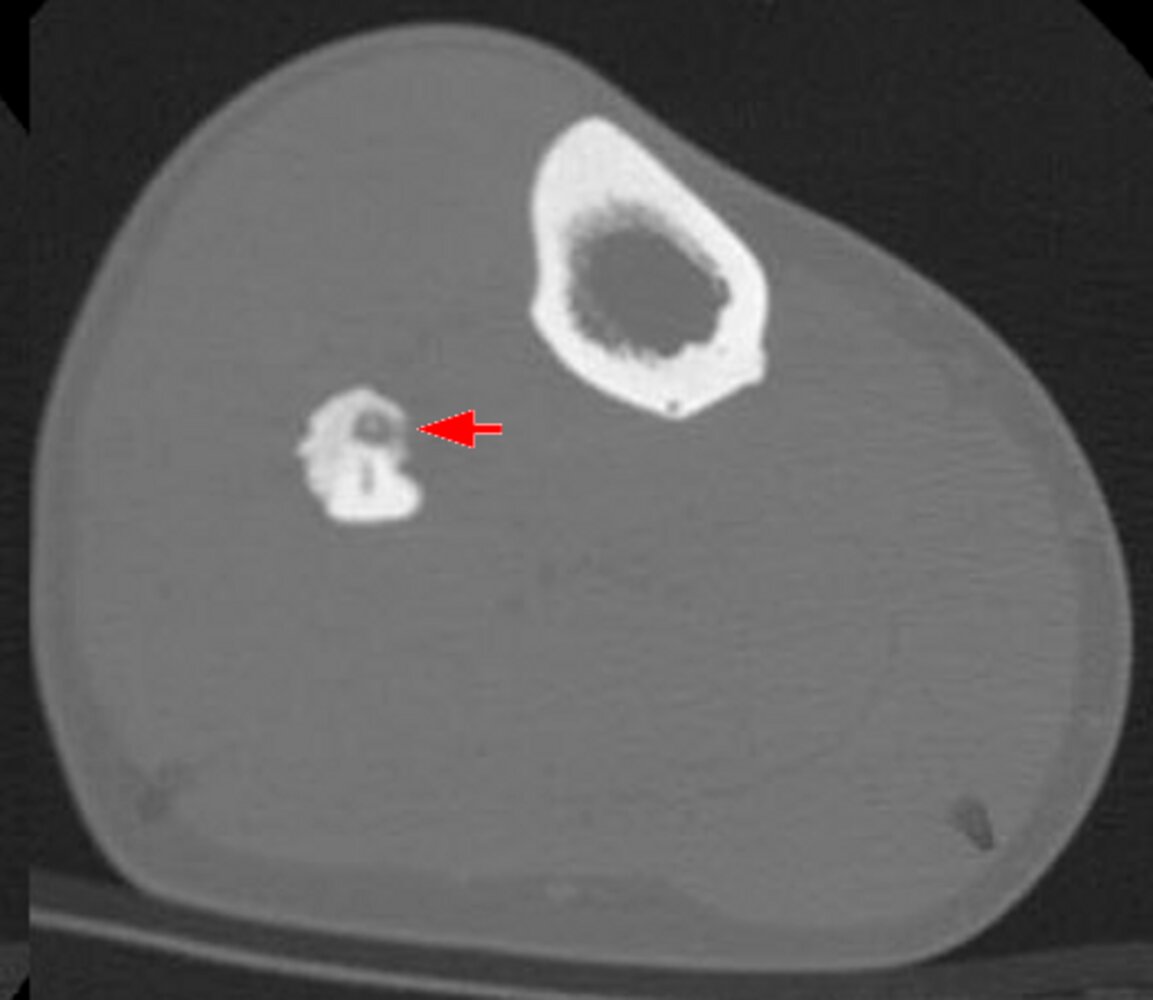
- X-ray or CT: radiolucent core (osteoid), surrounded by perifocal sclerosis (nidus)
-
Scintigraphy: usually intense enhancement
- Double-density sign
- Intraoperative nuclear imaging using a probe to detect the tumor
- Treatment: NSAIDs or surgical removal if pain is unresponsive to medical treatment


Osteoblastoma [6]
- Description: predominantly cortical tumor larger than osteoid osteoma (> 2 cm)
-
Epidemiology
- Peak incidence: 10–20 years
- Sex: ♂ > ♀
-
Clinical features
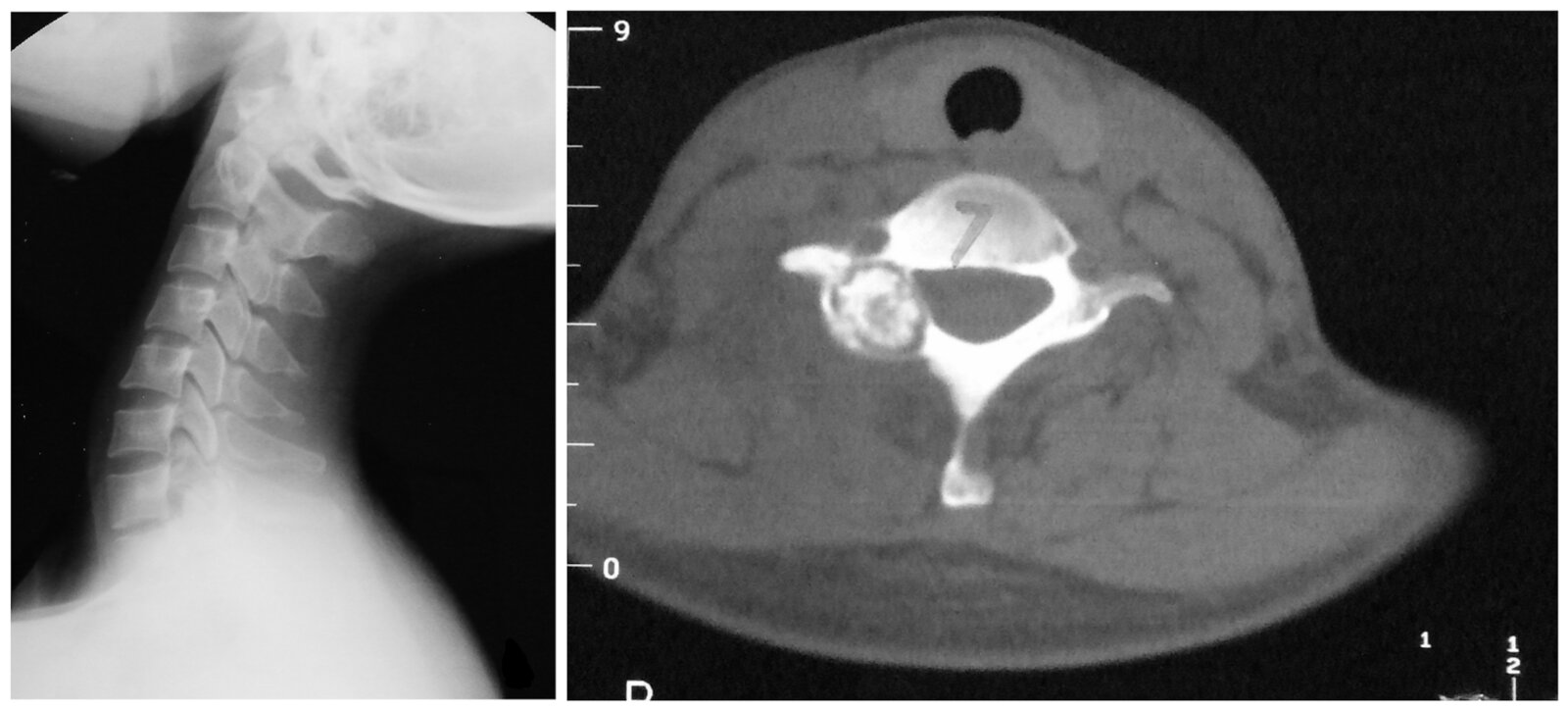
- Typically involves the posterior elements of the vertebrae (vertebral arch)
- Severe chronic local pain (no nocturnal pain) that does not respond to NSAIDs
- Neurologic symptoms if the spinal cord is compressed
-
Diagnostics: x-ray
- Shows tumor located in the cortical bone
- Central lucent nidus with mild or absent perifocal sclerosis
-
Treatment
- Unresponsive to NSAIDs
- Surgical curettage and bone grafting preferred
- Description: benign round bone tumor
- Epidemiology: most common in middle-aged individuals but may develop at any age
- Etiology: associated with Gardner syndrome
-
Clinical features
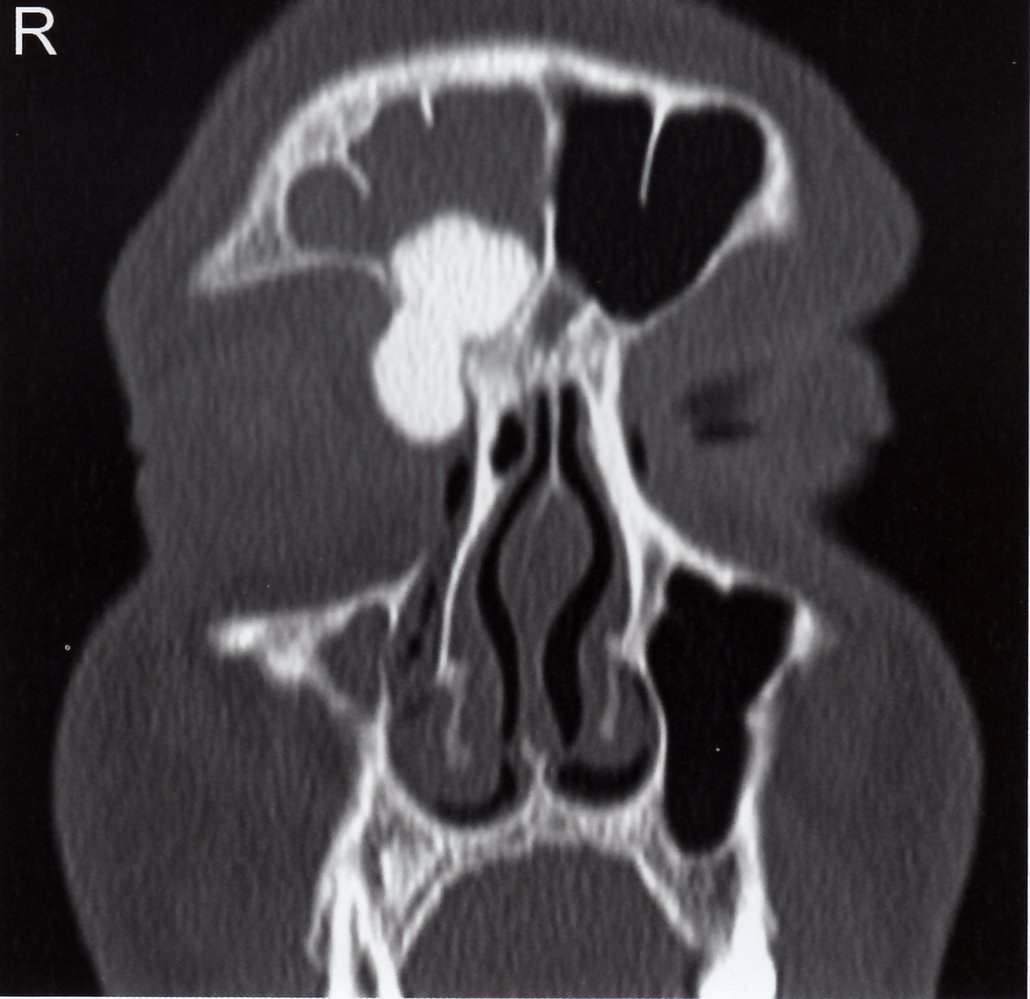
- Usually affects facial bones and cranial bones (most commonly affects paranasal sinuses)
- In rare cases, long bones
- Often asymptomatic
- An osteoma of the paranasal sinus may lead to obstruction of the ostium, with subsequent congestion and pressure headaches.
- Associated with Gardner syndrome: extracolonic manifestation of familial adenomatous polyposis (FAP) that includes osteomas of the skull or mandible, hypertrophy of the retinal pigment epithelium, adrenal adenomas, desmoid tumors, dental abnormalities, and cutaneous lesions
- Treatment: Surgical removal may be required if expansive tumor growth leads to symptoms.
Osteomas of the skull and mandible in conjunction with hypertrophy of the retinal pigment epithelium, adrenal adenomas, desmoid tumors, and dental abnormalities are characteristic of Gardner syndrome.
- Description: growth of fibrous connective tissue into areas that normally ossify; a tumor-like lesion that is considered to be a nonneoplastic disorder of bone growth, rather than a true neoplasm
- Epidemiology: peak incidence between 10 and 20 years
-
Clinical features
- Usually metaphyseal (predominantly in the distal femur and distal tibia)
- asymptomatic; usually an incidental finding[7][8]
-
Diagnostics: x-ray
- Marginal sclerosis
- Lobulated structure with translucent components
-
Treatment
- Usually self-limiting
- Bone grafting may be required for painful lesions or to prevent pathological fractures.



- Description: fibrous benign bone tumor
- Epidemiology: peak incidence between 1 and 5 years
-
Clinical features
- Most commonly found in tibia and fibula
- Localized swelling
- Tibial bowing
- Diagnostics: X-ray shows intracortical, osteolytic lesions with interspersed sclerosis.
-
Treatment
- If asymptomatic, monitoring is sufficient.
- If symptomatic, surgical removal is preferred.
- Description: Fibrous dysplasia is a benign, developmental disorder of bone that causes normal skeletal tissue to be replaced by fibrous tissue.
-
Epidemiology
- Fibrous dysplasia accounts for approx. 5% of benign bone lesions
- Age of onset: most commonly presents during adolescence
- Sex: ♂ = ♀
- Etiology: post-zygotically acquired, somatic, gain-of-function mutation in GNAS1 gene on chromosome 20q
-
Pathophysiology
- GNAS1 codes for the α subunit of the Gs protein (Gsα).
- Mutation → constitutive activation of certain Gs-cAMP coupled pathways → inhibition of mesenchymal differentiation into osteoblasts → lack of osteocytes → skeletal lesions composed largely of mesenchymal cells → weak, imperfect bone with fibrous tissue
-
Clinical features
- Disease phenotype
- Monostotic fibrous dysplasia (∼ 70% of cases)
- Polyostotic fibrous dysplasia (∼ 25% of cases)
- Common to all disease phenotypes
- Bone pain, bone deformities, and/or pathological fractures
- Entrapment neuropathies may occur as a result of expanding bone lesions
- Age at manifestation
- Monostotic fibrous dysplasia: 20–30 years
- Polyostotic fibrous dysplasia: < 10 years
- Disease phenotype
-
Diagnostics
- Laboratory tests
- ↑ Alkaline phosphatase (occasionally)
- Normal calcium, PTH, and 1,25-dihydroxyvitamin D levels
- Imaging: x-ray
- Long bones: well-defined, lobulated lesions with a thin cortex and a radiolucent, ground-glass appearance
- Facial bones: radiodense lesions with a leonine appearance
- Pathology: bone biopsy
- Laboratory tests
-
Therapy
- Bisphosphonates
- Management of precocious puberty: See “Peripheral precocious puberty.”
-
Prognosis
- The lesions do not heal spontaneously.
- Osteosarcomas occur in < 1% of cases.
References:[9]
Syndromes associated with polyostotic fibrous dysplasia
-
McCune-Albright syndrome
- Polyostotic fibrous dysplasia
- Café au lait spots with unilateral, ragged edges
- Most commonly peripheral precocious puberty
-
Mazabraud syndrome
- Polyostotic fibrous dysplasia
- Intramuscular myxomas
-
Jaffe-Lichtenstein syndrome
- Café au lait spots
- Polyostotic fibrous dysplasia

- Description: solitary, single-chambered cyst
- Epidemiology: peak incidence between 5 and 15 years
-
Clinical features
- Found in metaphysis of the long bones (predominantly the proximal humerus and proximal femur)
- Usually asymptomatic
- Pathological fractures
-
Diagnostics
- X-ray: osteolytic bone lesion with sharp margins and no sclerosis in the metaphysis of long bones
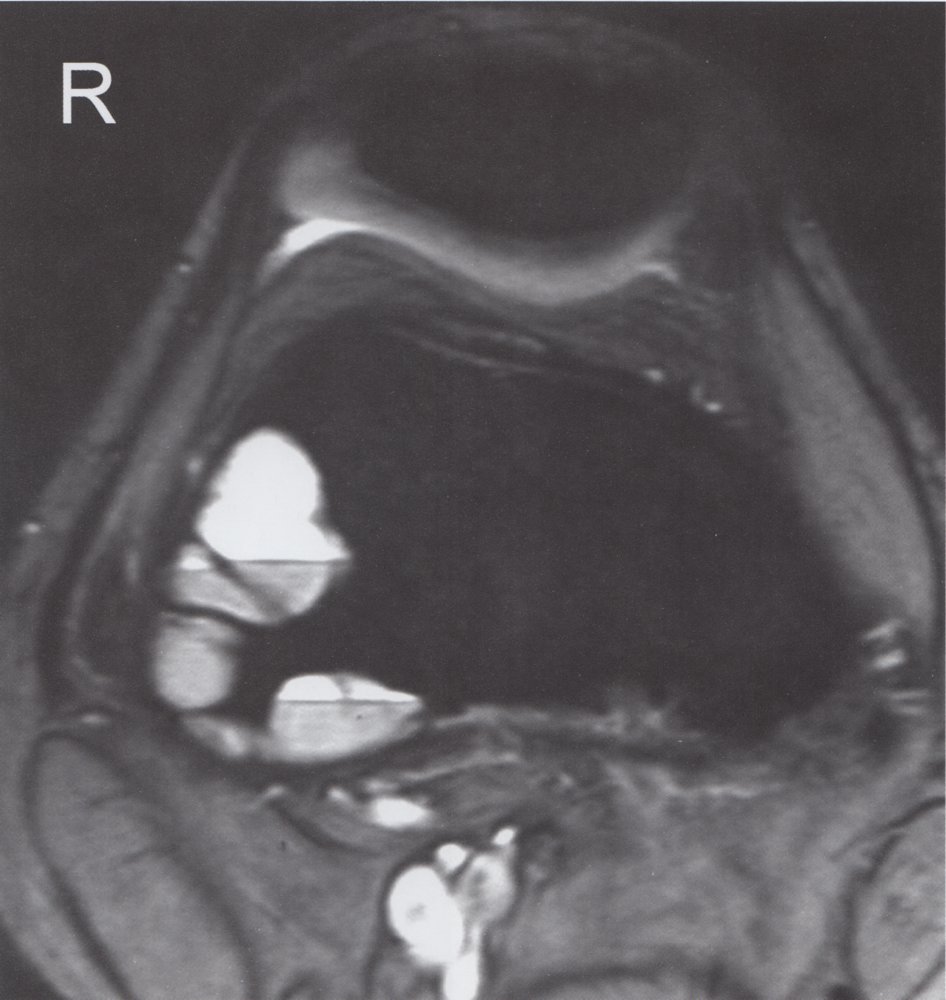
- MRI: single-chambered, fluid-filled lesion
- Treatment: monitoring or aspiration and corticosteroid injection for larger lesions
-
Description
- Osteolytic lesions; usually septated, blood-filled cysts
- Idiopathic (primary aneurysmal bone cyst) or secondary to malignant or other benign bone diseases (secondary aneurysmal bone cyst)
- Epidemiology: peak incidence between 10 and 20 years
-
Clinical features
- Common sites are the spine and the metaphysis of the femur and tibia.
- Usually asymptomatic; local pain and swelling may occur
- Pathological fracture: often the first sign
-
Diagnostics
- X-ray: metaphyseal, osteolytic lesion with sclerotic margins
- MRI : septated, blood-filled lesions, with typical fluid-fluid levels.
- Treatment: surgical curettage and bone grafting
- Prognosis: high risk of recurrence

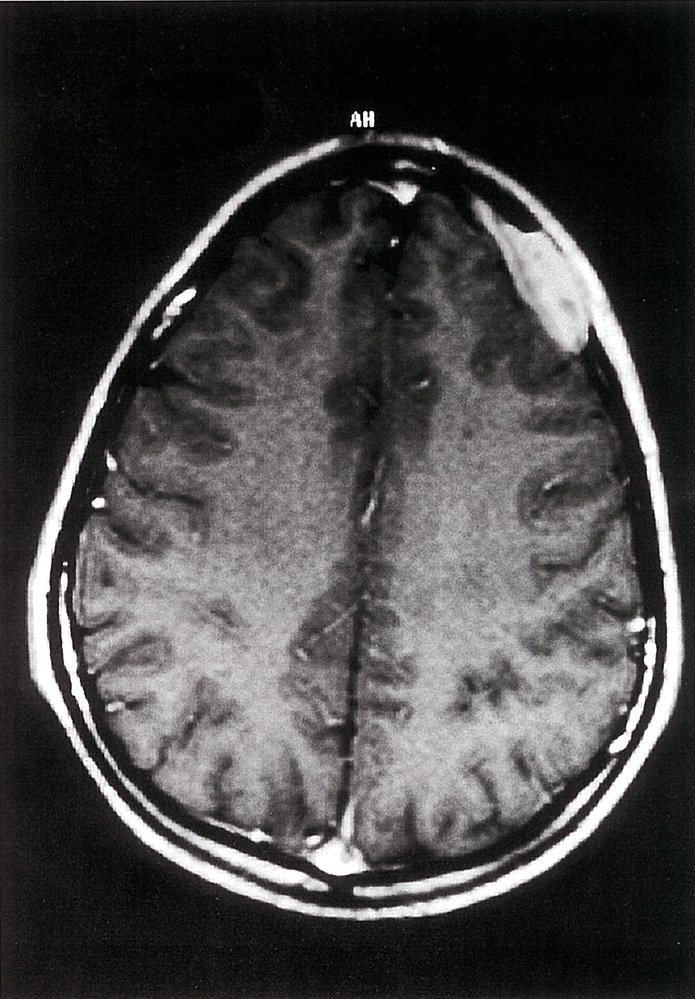
- Description: vascular neoplasm [10]
-
Epidemiology
- Peak incidence: 30–50 years
- Sex: ♂ < ♀ (1:2)
-
Clinical features
- Most common benign tumor of the spine, particularly in the thoracic and lumbar vertebrae
- Usually asymptomatic; often an incidental finding
-
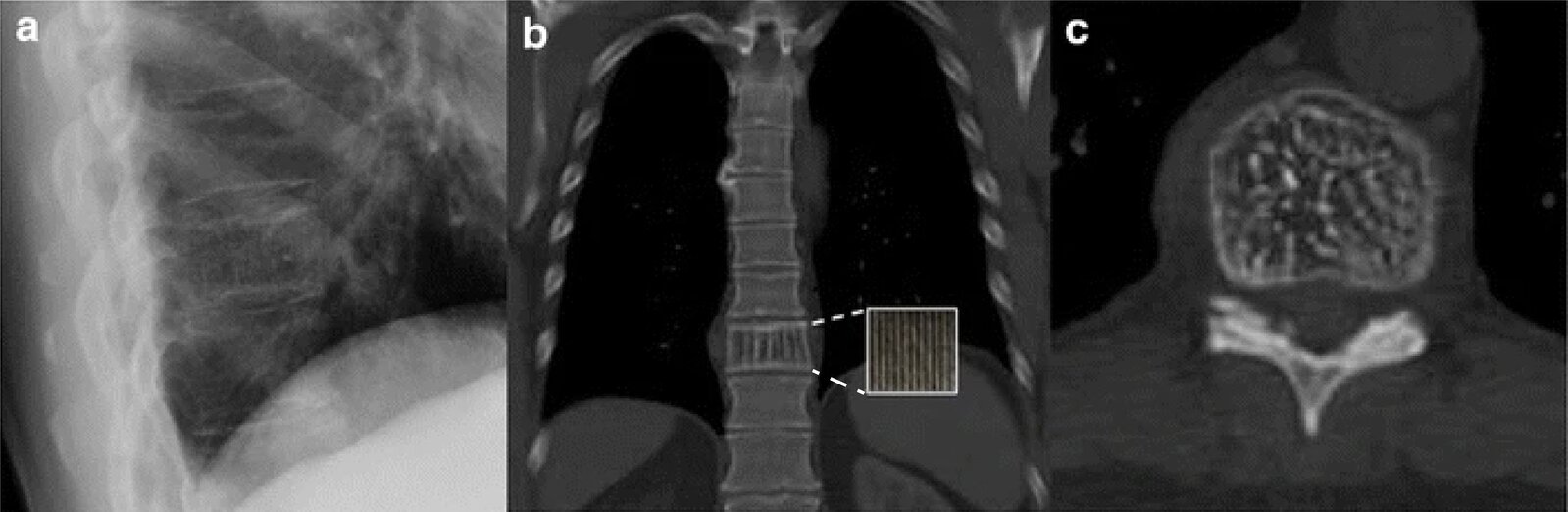
Diagnostics: x-ray
- Vertical streaks visible in vertebrae
- Honeycomb appearance of lesion with sharp margins
- Treatment: usually no treatment required
-
Complications
- Compression fractures
- Spinal stenosis
- Bleeding with subsequent spinal epidural hematoma

- Description: : a rare disorder caused by clonal proliferation of Langerhans cells (antigen-presenting cells) [11]
- Epidemiology: : peak incidence between 5 and 10 years
-
Clinical features
-
Osseous lesions (90%): pain and/or swelling, pathological fractures
-
Localization: skull (most common site), femur, vertebra, mandible, ilium, ribs
- Can cause recurrent otitis media if the mastoid bone is involved
- Unifocal or multifocal
-
Localization: skull (most common site), femur, vertebra, mandible, ilium, ribs
- Systemic manifestations (less common)
- Skinrash: brown to purple papules and/or eczematousrash
- Hepatomegaly and/or splenomegaly
- Lymphadenopathy
- Bone marrow infiltration
- Hypopituitarism that typically manifests as central diabetes insipidus
- Exanthema
-
Osseous lesions (90%): pain and/or swelling, pathological fractures
-
Diagnostics
- Normal calcium levels
- X-ray: osteolytic lesions with or without marginal sclerosis
-
Biopsy (confirmatory test): proliferation of Langerhans cells (polygonal cells with coffee bean-shapednucleiand eosinophilic cytoplasm) ; [12][13]
- Electron microscopy: Birbeck granules (tennis racket-shaped or rod-like structures) in the cytoplasm
- Immunohistochemistry: cells are positive for S100, CD1a, and/or CD207
-
Treatment
- Solitary bone lesions in low-risk anatomical regions
- Asymptomatic lesion: a wait-and-watch approach may be appropriate
- Symptomatic lesion: curettage and/or excision (as a part of biopsy)
- Bone lesions in high-risk anatomical regions (e.g., lesions involving the odontoid process or regions of the skull other than the vault), multifocal bone involvement, or systemic manifestation: vinblastine and prednisone
- Solitary bone lesions in low-risk anatomical regions