Botulism is an acute paralytic disorder caused by exposure to botulinum neurotoxin produced by Clostridium botulinum. The most common forms are foodborne botulism, infant botulism, wound botulism, and iatrogenic botulism. Clinical features include cranial nerve palsies, neuromuscular weakness or paralysis, and autonomic nervous system dysfunction. Botulism is a clinical diagnosis later confirmed based on detection of botulinum neurotoxin or C. botulinum in collected specimens. Management focuses on airway management and preventing the progression of paralysis by administering botulism antitoxin therapy. All patients are admitted to the ICU for supportive care and monitoring.
Etiology [1]
-
Pathogen: C. botulinum
- Gram-positive rod
- Spore-forming
- Obligate anaerobe
- Toxin: botulinum neurotoxin (heat-labile)
-
Route of exposure: ingestion, colonized wound, or local injections
- Foodborne botulism: caused by ingestion of botulinum neurotoxin from contaminated food
- Infant botulism: caused by ingestion of endospores from the environment, leading to in vivo production of botulinum neurotoxin
- Wound botulism: caused by contamination of a wound, resulting in production of botulinum neurotoxin
- Iatrogenic botulism: caused by excessive injection of botulinum neurotoxin
- Adult colonization botulism (rare): similar to infant botulism
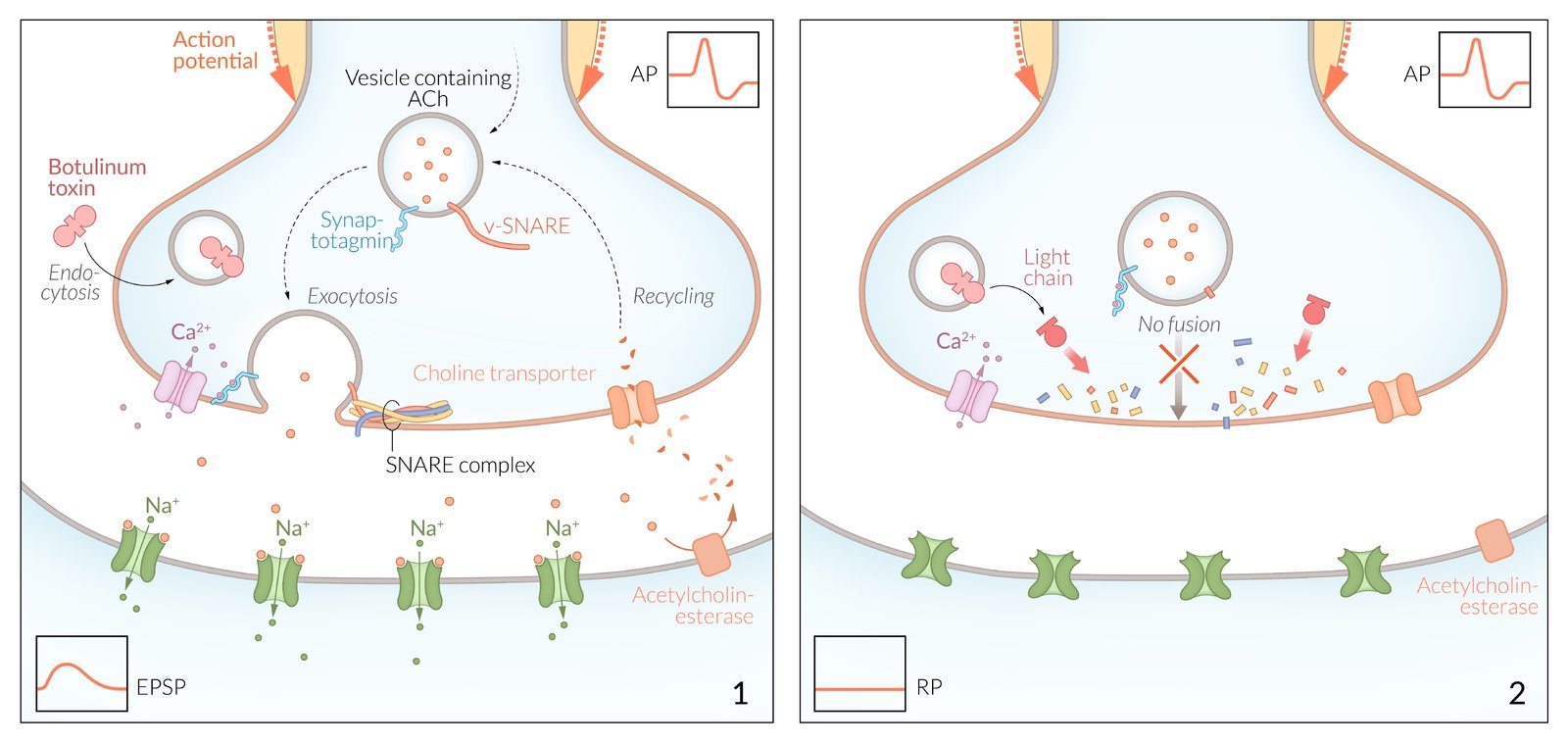
Pathophysiology [2]
Botulinum neurotoxin (a protease) cleaves SNARE proteins → prevention of neurotransmitter-containing vesicles fusing with the presynaptic membrane → inhibition of acetylcholine release from the presynaptic axon terminals → flaccid muscle paralysis
Clinical features of botulism [1][3]
-
Cranial nerve palsies (> 90% of patients) [3]
- Ptosis
- Ophthalmoplegia (e.g., mydriasis, loss of visual accommodation, diplopia)
- Dysarthria, dysphagia
-
Muscle weakness or paralysis
- Symmetrical descendingmuscle weakness or paralysis
- Affects proximal muscles more than distal muscles
- Respiratory muscle involvement may cause dyspnea and respiratory failure.
-
Autonomic nervous system dysfunction
- Xerostomia
- Urinary retention
- Constipation, ileus
Cranial nerve palsies are the most common early feature of botulism; suspect an alternative diagnosis in patients with no or late onset of cranial nerve palsies. [4]
Five D's of botulism: Dysarthria, Diplopia, Dysphagia, Dyspnea, and Descending paralysis.
Diagnosis of botulism [1][5]
Botulism is a clinical diagnosis; diagnostic confirmation may take 24–48 hours. [1]
-
Diagnosis is confirmed if botulinum neurotoxin or C. botulinum are detected in collected specimens.
- Foodborne or infant botulism: serum, gastric fluid, stool, suspected food
- Wound botulism: serum, wound specimen
- Routine laboratory studies (e.g., CBC, CSF analysis) and imaging studies are typically normal.
- Electrodiagnostic studies (e.g., EMG, repetitive nerve stimulation) may help differentiate botulism from other paralytic diseases.
- See also “Diagnostics for neuromuscular weakness.”
If botulism is suspected in the US, contact the state health department and CDC to discuss specimen collection and testing. [1]
Differential diagnoses [1][4]
- Guillain-Barré syndrome
- Myasthenia gravis
- Lambert-Eaton myasthenic syndrome
- Tick paralysis
- Poisoning (e.g., cholinergic poisoning, puffer fish poisoning)
- Stroke
- Poliomyelitis
- See also “Acute or rapidly progressive causes of neuromuscular weakness.”
Suspect botulism if ≥ 2 patients present with clinical features compatible with botulism; other illnesses with these features do not typically occur in outbreaks. [4]
Management of botulism [1]
- Monitor for signs of respiratory failure and provide respiratory support in botulism as needed.
- Consult infectious diseases and local health department.
-
Administer botulism antitoxin therapy for all suspected cases under specialist guidance.
- Noninfant botulism: Botulism antitoxin (equine)
- Infant botulism: Botulism immune globulin (BabyBIG)
- Treat complications (e.g., NG tube for ileus and/or Foley catheter for urinary retention).
- Avoid medications that may worsen the paralysis.
- Admit all patients to the ICU.
In infants with suspected foodborne botulism (e.g., part of a botulism outbreak), treat for foodborne botulism rather than infant botulism. [1]
Botulinium antitoxin neutralizes neurotoxin that has not yet bound to a synaptic receptor; it cannot reverse existing paralysis. [1]
Respiratory support in botulism [1]
- Perform serial spirometry and respiratory muscle function testing.
- Consider mechanical ventilation for any of the following:
- Forced vital capacity < 20 mL/kg
- Maximal inspiratory pressure < 30 cm H2O
- Maximal expiratory pressure < 40 cm H2O
- Use ventilation strategies for neuromuscular weakness.
- Provide adjunctive care of ventilated patients as needed.
-
Etiology [1]
-
Ingestion of preformed botulinum neurotoxin from contaminated foods
- Endospores survive in foods that have been inadequately pasteurized.
- Germinated endospores produce botulinum neurotoxins and gas.
- Common sources include home-canned or processed foods (e.g., fish, vegetables, tofu, dairy products). [6]
-
Ingestion of preformed botulinum neurotoxin from contaminated foods
- Incubation period: 12–36 hours [7]
-
Clinical features [8]
- Clinical features of botulism
- Nausea, vomiting, abdominal pain, and diarrhea may be present. [8]
- Diagnosis: See “Diagnosis of botulism.”
-
Management
- See “Management of botulism.”
- Gastrointestinal decontamination may clear residual neurotoxins but is not supported by evidence. [5][9]
-
Prevention [8]
- Following approved heating processes for canning food (e.g., pressure cooker)
- Discarding all canned foods that appear swollen, damaged, or abnormal
C. botulinum produces gas that may cause cans of contaminated food to bulge. [6]
- Epidemiology: peak incidence between 6 weeks and 6 months old [5]
-
Etiology
- Ingestion of endospores from the environment (e.g., honey, soil, juice)
- Endospores germinate in the intestine and produce botulinum neurotoxin.
- Incubation period: 3–30 days [10]
-
Clinical features ; [5]
- Constipation
- Poor feeding
- Weak cry
- Loss of head control
- Hypotonia
- Other clinical features of botulism (e.g., ptosis)
- Differential diagnosis: See “Differential diagnosis of infantile hypotonia.”
- Diagnosis: See “Diagnosis of botulism.”
- Management: See “Management of botulism.”
- Prevention: avoiding honey in children < 1 year of age [10]
Do not wait for diagnostic confirmation to begin treatment of infant botulism. [10]

| Differential diagnosis of infantile hypotonia [11] | |||
|---|---|---|---|
| Condition | Etiology | Clinical features | Management |
| Infant botulism |
|
|
|
| Neonatal myasthenia gravis |
|
|
|
| Spinal muscular atrophy type 1 |
|
|
|
| Myotonic dystrophy type 1 |
|
|
|
| Trisomy 21 |
|
|
|
-
Etiology [10]
- Contamination of a wound by C. botulinum, resulting in production of botulinum neurotoxin
- Typically associated with trauma or IV drug use
- Incubation period: 4–14 days [10]
-
Clinical features
- Clinical features of botulism
- Potential signs of wound infection
- Diagnosis: See “Diagnosis of botulism.”
-
Management [5]
- See “Management of botulism.”
- Consult surgery for wound debridement.
- Consider antibiotic therapy for skin and soft tissue infections for concurrent infections.
-
Prevention
- Avoiding IV drug use
- Appropriate management of acute wounds
-
Etiology [12]
- Excessive therapeutic or cosmetic injection of botulinum neurotoxin
- Botulinum neurotoxin may be used to treat muscle spasms, focal dystonia, hyperhidrosis, or facial wrinkles.
- Management: See “Management of botulism.”