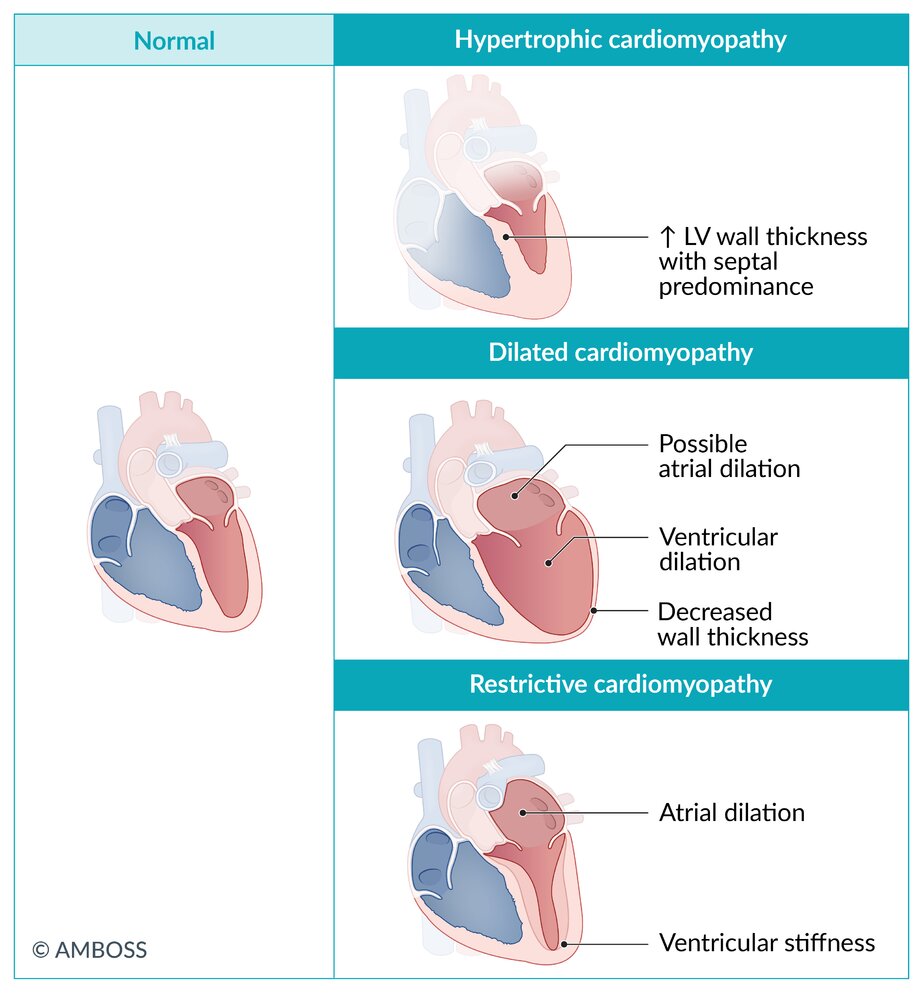
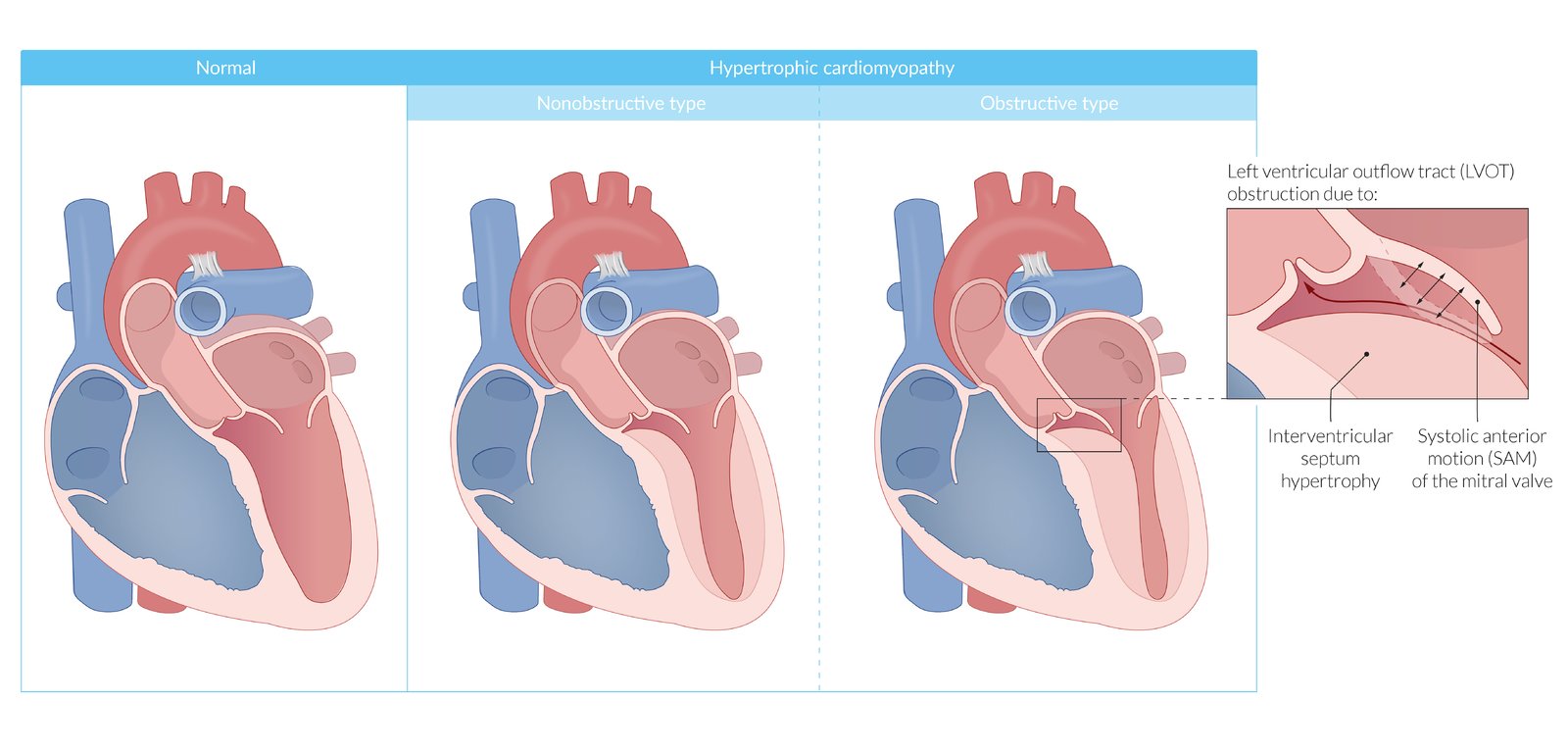
Cardiomyopathies are diseases of the muscle tissue of the heart. Types of cardiomyopathies include dilated (most common), hypertrophic, restrictive, and arrhythmogenic right ventricular cardiomyopathy.
Arrhythmogenic right ventricular cardiomyopathy (ARVC) primarily affects the right ventricle and is characterized by fibrofatty replacement of myocardium, which causes myocardial thinning and subsequent ventricular dilation. Although the hallmark finding is arrhythmia, symptoms are highly variable. Because management depends greatly on individual factors, such as the extent of the disease, there is no single best course of treatment. All patients should avoid strenuous exercise.
Arrhythmia-induced cardiomyopathy is a very rare type of cardiomyopathy. It is caused by long-standing arrhythmia and typically affects the left ventricle. Features include palpitations, syncope, and signs of arrhythmia on ECG. Progression to left heart failure is possible in severe cases. Treatment involves antiarrhythmics such as beta blockers for rhythmic control.
“Dilated cardiomyopathy”, “Hypertrophic cardiomyopathy,” “Restrictive cardiomyopathy,” and “Peripartum cardiomyopathy” are described in their respective articles in more detail.
| Differential diagnosis of major cardiomyopathies | ||||
|---|---|---|---|---|
| Types | Dilated cardiomyopathy | Hypertrophic cardiomyopathy | Restrictive cardiomyopathy | |
| Etiology |
|
|
|
|
| Pathophysiology |
|
|
|
|
| Distinctive clinical features |
|
|
|
|
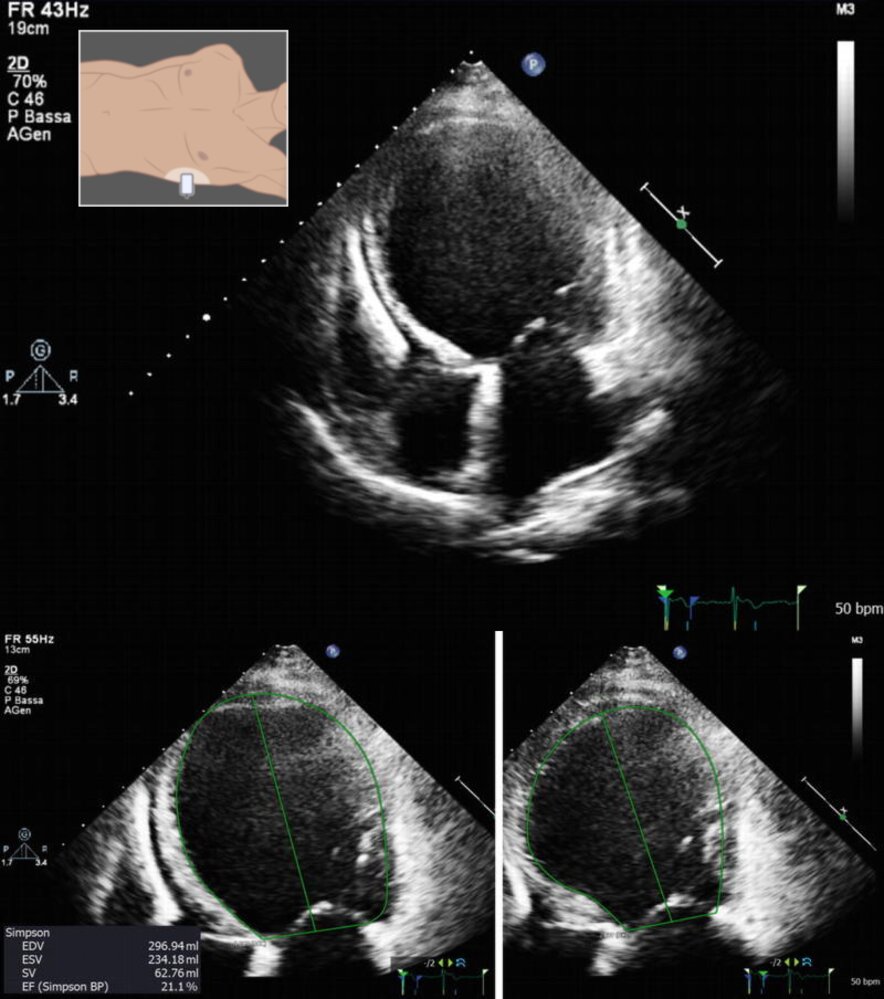
| Echocardiography | LV cavity size |
|
|
|
| EF |
|
|
|
|
| Wall thickness |
|
|
|
|
| Additional findings |
|
|
|
|
| Other characteristics |
|
|
|
|


Epidemiology
- Most common in young adults (mean age at diagnosis: ∼ 30 years) [2]
- Prevalence: 1:1,000–2,000 [3]
Etiology
- Mutations of various genes (e.g., JUP gene)
- Autosomal recessive or autosomal dominant inheritance [3][4]
Pathophysiology
- Right ventricularmyocardial celldeath (due to myocyteapoptosis, inflammation, and fatty/fibrotic tissue replacement) →thinning of the right ventricular wall → dilation of the ventricle → ventricular arrhythmia and dysfunction [2]
- The left ventricle can also be affected, but consequences are usually less severe.

Clinical features
- Highly variable
- Many patients remain asymptomatic.
- Angina pectoris
- Dyspnea
- Peripheral edema, ascites, hepatic and splenic congestion
- Palpitations, syncope, possibly sudden cardiac death (particularly during or after exercise)
Diagnostics [2][3][5]
Approach
ARVC is diagnosed based on the AHA criteria which include the following features:
- Dysfunction and structural abnormalities of RV (can be revealed by echocardiography, MRI, or RV angiography)
- Histological characteristics (require myocardial biopsy)
- Abnormal repolarization (diagnosed with ECG)
- Depolarization/conduction abnormalities (diagnosed with ECG)
- Arrhythmias (diagnosed with ECG)
- Family history (confirmation of ARVC in a relative either by criteria, pathological examination in surgery or autopsy, or by genetic testing)
Findings
-
ECG
-
Repolarization disturbances in the right precordial leads (V1-3)
- Possibly epsilon wave (at the end of a widened QRS complex)
- Highly specific for ARVC but only occurs in ∼ ⅓ of patients
- Increased QRS duration
- Ventricular tachycardia
- Ventricular extrasystoles
-
Repolarization disturbances in the right precordial leads (V1-3)
-
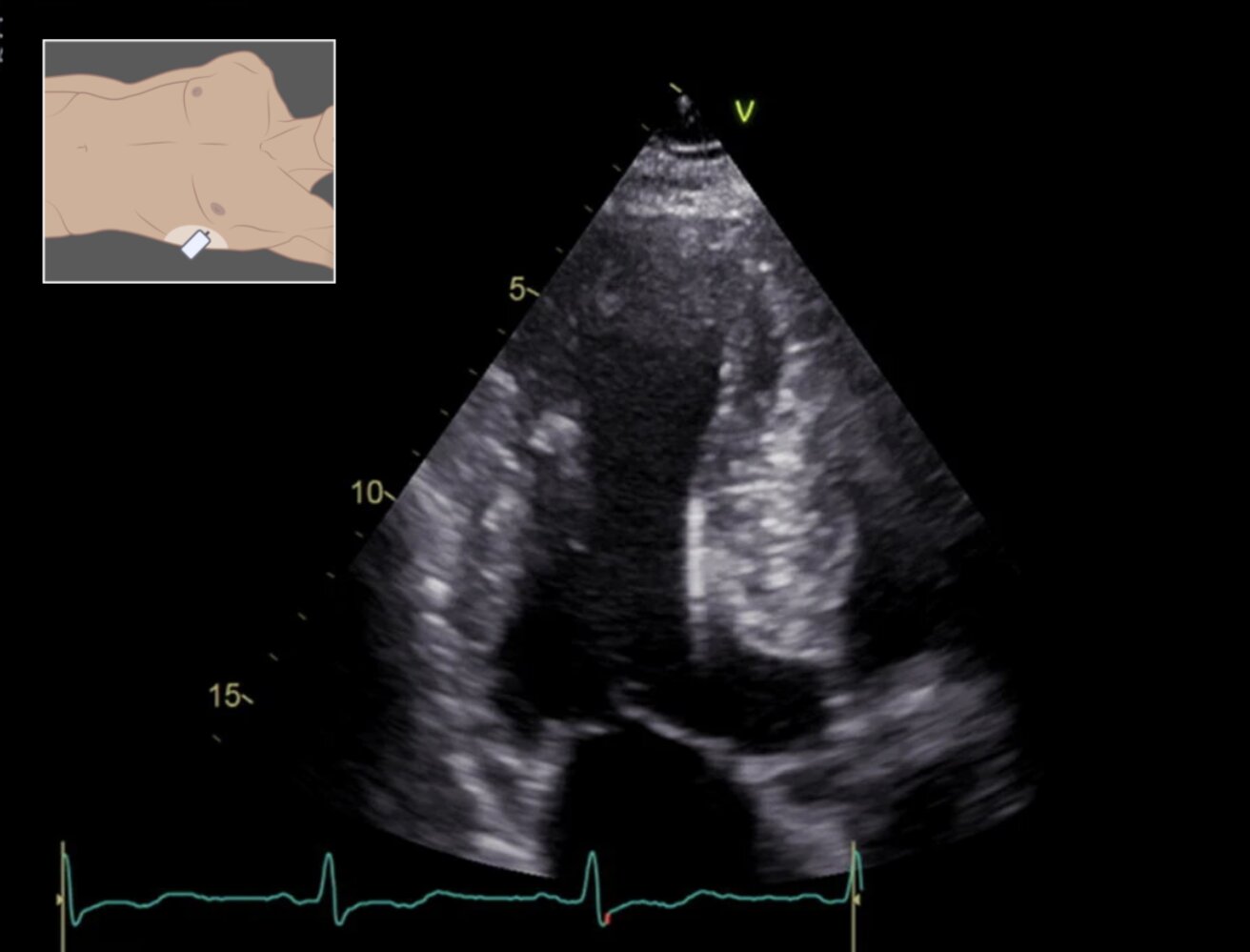
Echocardiography and cardiac MRI
- RV enlargement
- RV wall motion abnormalities
- ↓ RV EF
- Localized RV aneurysms
- Endomyocardial biopsy: fibrofatty replacement of myocardial tissue
- Genetic testing: Multiple genetic abnormalities that can cause ARVC have been identified (e.g., plakoglobin (JUP), desmoplakin (DSP), plakophilin-2 (PKP2), desmoglein-2 (DSG2), desmocollin (DSC2)). [4]

Management [5]
- Avoid intense physical exertion.
-
Antiarrhythmic treatment
- Pharmacologic: beta blockers (e.g., sotalol), amiodarone, calcium channel blockers
- Invasive
- AICD implantation (in high-risk patients, e.g., patients with left ventricular involvement)
- Radiofrequency ablation (only as ancillary treatment)
- Heart transplant (in severe cases that are refractory to all other treatments)
- Screening and genetic counseling for first-degree relatives [6]
Left ventricular noncompaction [7]
- Definition: rare inherited cardiomyopathy which is associated with structural abnormalities of the left ventricular myocardium (prominent trabeculations and deep intertrabecular recesses)
-
Clinical findings
- Signs of heart failure and arrhythmia (e.g., dyspnea, edema, chest pain, palpitations, syncope)
- Thromboembolisms
- Diagnostics: echocardiography and/or cardiac MRI: LV wall thickening, prominent trabecular meshwork, detection of abnormal flow (within the deep intertrabecular recesses)
-
Treatment: no causal treatment available
- Avoid intense physical exertion
- Symptomatic treatment of complications (e.g., heart failure)
- Prevention of thromboembolism
- AICD
- Heart transplant
- Family and genetic counseling
Arrhythmia-induced cardiomyopathy [8][9]
- Definition: recurring or persistent atrial or ventricular arrhythmias causing structural cardiac changes and left ventricular dysfunction (potentially reversible)
-
Etiology
- Supraventricular tachyarrhythmias (i.e., tachycardia, atrial fibrillation, atrial flutter, supraventricular reentry tachycardia)
- Ventricular tachyarrhythmia (less commonly than supraventricular tachyarrhythmias)
- Atrial or ventricular ectopy (with or without tachycardia)
-
Clinical features
- Signs of underlying arrhythmia (e.g., palpitations, syncope)
- Signs of left heart failure (e.g., dyspnea, chest pain, pulmonary edema)
-
Diagnostics
- ECG: tachyarrhythmia, ectopic foci
- Cardiac monitoring (e.g., Holter monitor)
- Echocardiography and/or cardiac MRI: to evaluate cardiac structure and function (e.g., LVEF measurement)
- To exclude other causes (e.g., coronary heart disease via coronary angiography)
-
Treatment
- Beta blockers: management of CHF, rate control in tachyarrhythmias
- Antiarrhythmics (e.g., amiodarone): rhythm control in tachyarrhythmias
- Catheter ablation: rhythm control in tachyarrhythmias, ectopic foci