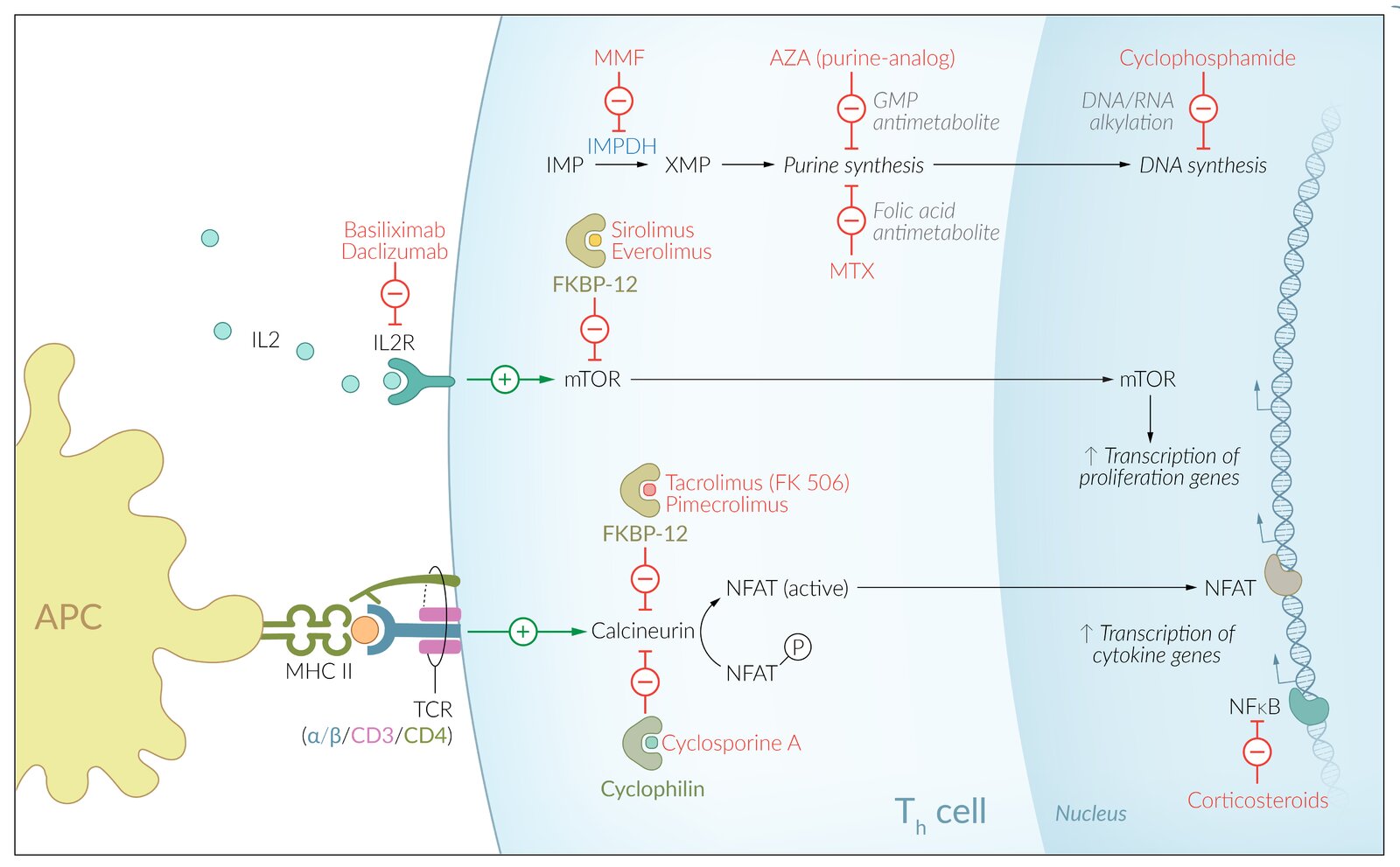
Immunosuppressants use heterogeneous mechanisms of action to suppress the body's cell-mediated and humoral immune response. They may be used as transplant rejection prophylaxis or to treat autoimmune disorders such as lupus, psoriasis, and rheumatoid arthritis. Commonly used immunosuppressants include cyclosporine A, tacrolimus, glucocorticoids, methotrexate, and biological agents (e.g., rituximab). A common side effect of immunosuppressants is an increased susceptibility to infection and malignancy.
Glucocorticoids are discussed in detail in another article.
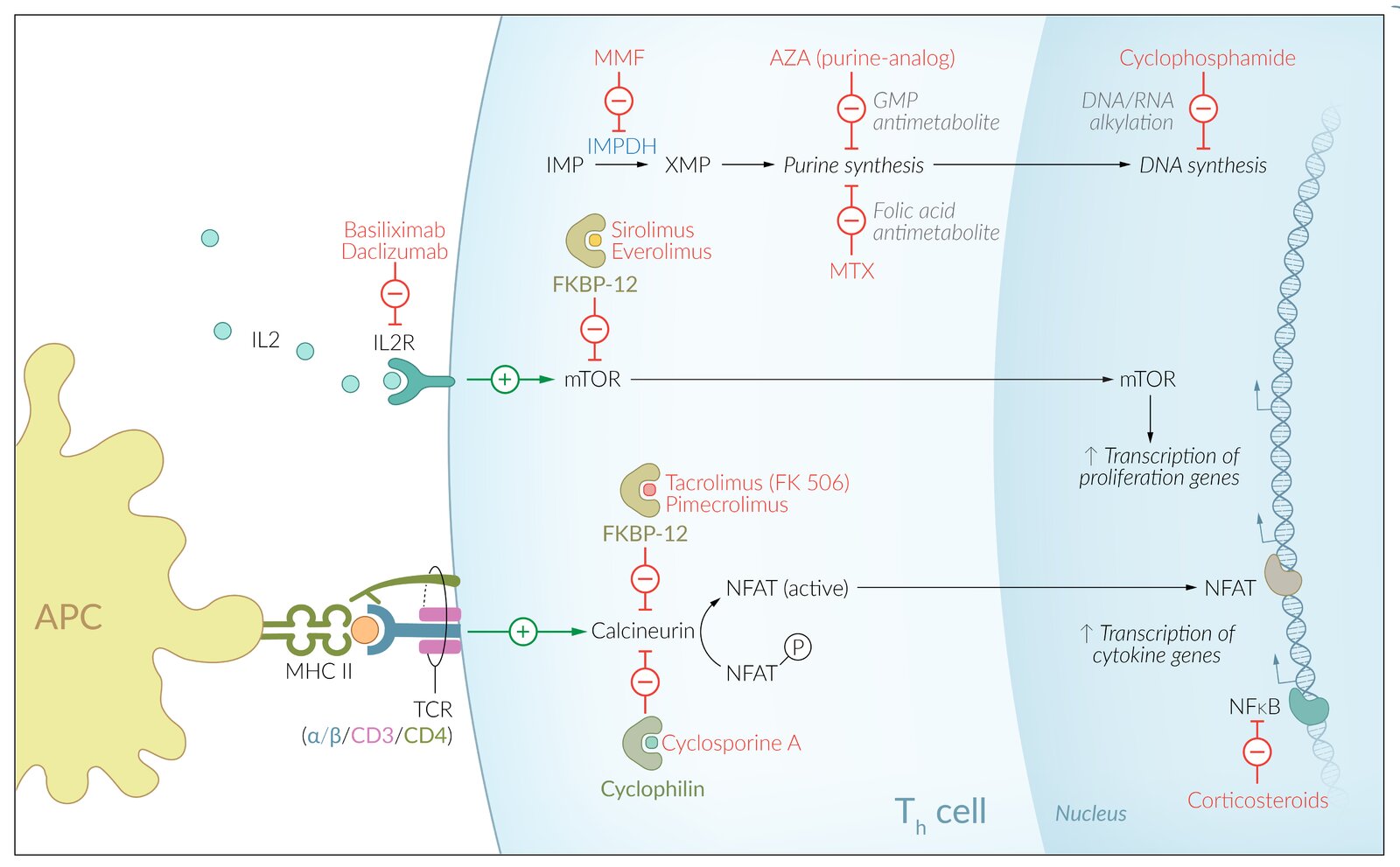
- Immunosuppressants are a heterogeneous class of drugs used to suppress the body's cell-mediated and humoral immune response via lymphocyte inhibition.
- The most common indications include transplant rejection prophylaxis and the treatment of autoimmune disorders such as lupus, psoriasis, and rheumatoid arthritis.
- It is common practice to use a combination of different immunosuppressive drugs to maximize their immunosuppressive effect and minimize their side effects.
- A common side effect of long-term immunosuppressants use is an increased susceptibility to infection and malignancy.
| Overview of immunosuppressants | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Immunosuppressant class | Common drugs | Mechanism of action | Suppression of cell-mediated immune response | Suppression of humoral immune response | Indications | Adverse effects | |||||
| Glucocorticoids | Prednisolone, hydrocortisone, dexamethasone |
|
|
|
|
|
|||||
| Calcineurin inhibitors (calcineurin =calcium- and calmodulin-dependentserine-threoninephosphatase) | Cyclosporine A |
|
|
|
|
|
|
||||
| Tacrolimus (also FK-506 or fujimycin) |
|
|
|
|
|
||||||
| Pimecrolimus |
|
||||||||||
| mTOR inhibitors | Sirolimus (also known as rapamycin) |
|
|
|
|
|
|
||||
| Everolimus [1] |
|
||||||||||
| Purine analog | Azathioprine (mercaptopurine) |
|
|
|
|
|
|||||
| IMDH/IMPDH inhibitors | Mycophenolate mofetil |
|
|
|
|
|
|||||
| Other cytostatic and antiproliferative agents | Methotrexate [3] |
|
|
|
|
|
|||||
| Cyclophosphamide |
|
|
|
|
|
||||||
| Protein drugs | Antibodies |
|
|
|
|
||||||
| Other biological proteins | |||||||||||
| ✓ = Definite suppression (✓) = Probable suppression (inconclusive research currently) – = No suppression | |||||||||||
- Biological agents are recombinant proteins that intervene in immunological processes.
- Used in autoimmune diseases and malignancies
- Although complex and costly, they can significantly improve the success of treatment in some cases.
- The naming of antibodies follows a certain classification scheme:
- The suffix "-mab": indicates "monoclonal antibody."
- Second to last syllable: describes the origin (e.g., "xi"=chimeric, "u"=human)
- Third to last syllable: denotes the target (e.g., li(m)=immune system)
| Overview of biologics | ||||||
|---|---|---|---|---|---|---|
| Antibody | Type | Target | Indication | Adverse effects | ||
| Infliximab |
|
|
|
|
|
|
| Adalimumab |
|
|||||
| Golimumab | ||||||
| Certolizumab | ||||||
| Etanercept |
|
|||||
| Rituximab |
|
|
|
|
||
| Natalizumab |
|
|
|
|||
| Cetuximab |
|
|
|
|
||
| Panitumumab |
|
|||||
| Tocilizumab |
|
|
|
|||
| Palivizumab |
|
|
|
|||
| Secukinumab |
|
|
|
|||
| Ixekizumab |
|
|||||
| Brodalumab |
|
|
|
|||
| Vedolizumab |
|
|
|
|||
| Ustekinumab |
|
|
|
|||
| Omalizumab |
|
|
|
|
||
| Abciximab |
|
|
|
|
||
| Muromonab-CD3 |
|
|
|
|
||
| Basiliximab |
|
|
|
|
||
| Daclizumab |
|
|||||
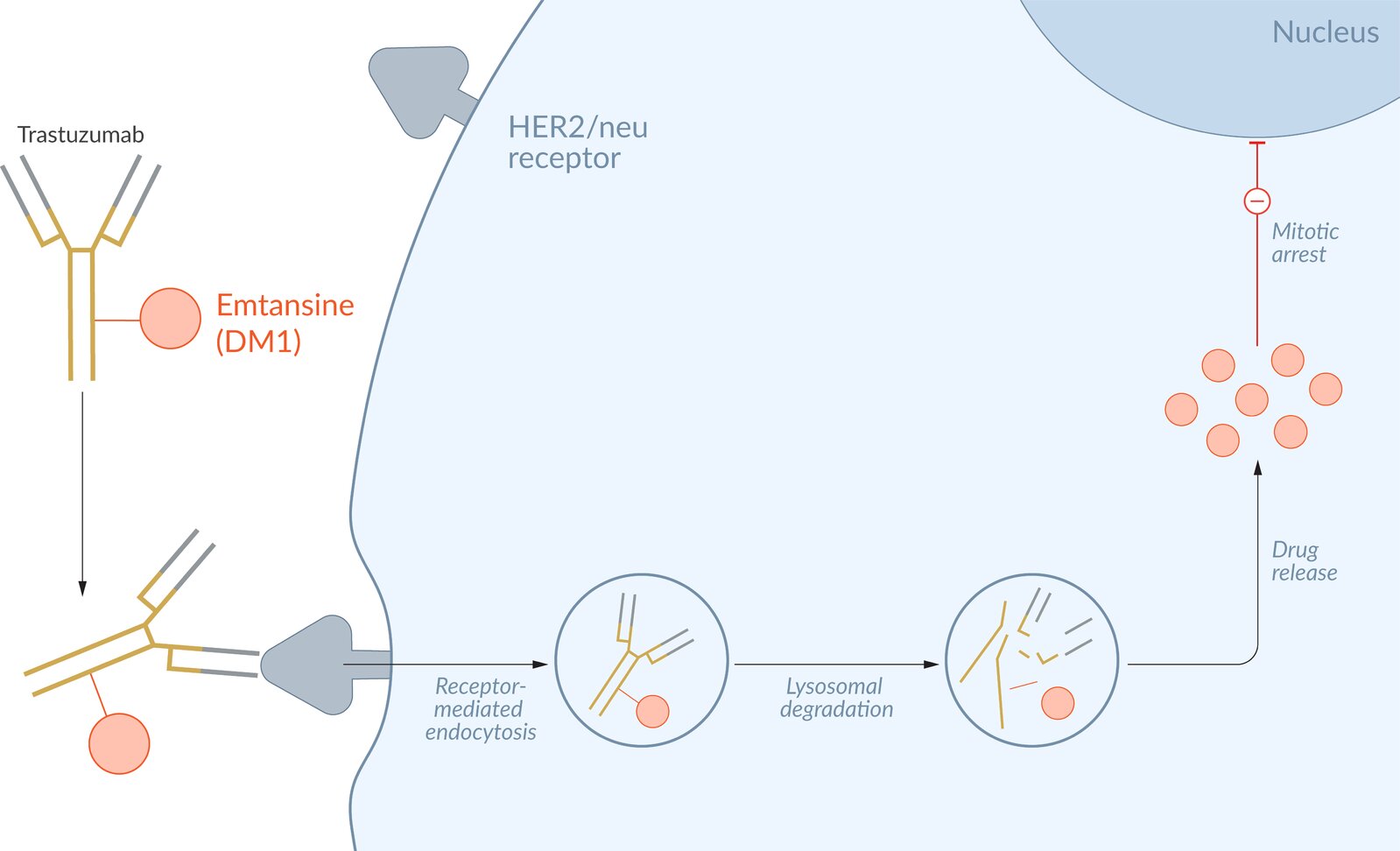
| Trastuzumab |
|
|
|
|
||
| Bevacizumab |
|
|
|
|
||
| Eculizumab |
|
|
|
|
||
| Denosumab |
|
|
|
|
||
| Alemtuzumab |
|
|
|
|
||
| Guselkumab |
|
|
|
|||
|
|
|||||
| Ipilimumab |
|
|
||||
| Pembrolizumab |
|
|
|
|||
| Nivolumab |
|
|||||
| Cemiplimab | ||||||
| Avelumab |
|
|||||
| Durvalumab | ||||||
| Atezolizumab |
|
|||||
“BeVAcizumab Blocks VAsculature: bevacizumab inhibits angiogenesis”
For the most important indication (breast cancer) and the target ERBB2 (HER2) of trastuzumab, think “Her two (HER2) breasts can be treated with trastwozumab.”
To remember the indication for alemtuzumab, think “ALYMtuzumab for chronic LYMphocytic leukemia.”
Calcineurin inhibitors
- Calcineurin inhibitors become even more neurotoxic and nephrotoxic when combined; for this reason, they should never be coadministered.
- Because of their neurotoxicity, patients receiving higher doses and those who have decreased renal function should be closely monitored.
Calcineurin inhibitors frequently induce endothelial injury and arteriolar vasoconstriction, causing a variety of toxicities. [5]
Cyclosporine A
- Nephrotoxicity
- Neurotoxicity
- Gingival hyperplasia
- Hypertrichosis and hirsutism
-
Diabetogenic effect (particularly after organ transplantation), which can lead to:
- Hyperuricemia
- Hyperlipidemia
- Elevated liver enzymes
- Increase in malignancies and infectious diseases (e.g., increase in the risk of squamous cell carcinoma by 50% in patients who are on simultaneous treatment with PUVA during psoriasis treatment)
- Hypertension
- Hyperkalemia
- Tremors
- Nausea and diarrhea
Tacrolimus (FK506) [6]
- Nephrotoxicity: monitor for oliguria
- Neurotoxicity (more severe compared to cyclosporin)
- Hypertension
-
Diabetogenic effect (more severe compared to cyclosporin A) ; [7]
- Hyperglycemia
- Hyperuricemia
- Hyperlipidemia
- Elevated liver enzymes
- Hair loss
- Headache
- Nausea and diarrhea
- Insomnia
- Abdominal discomfort
- Hyperkalemia
- Hypophosphatemia
- Hypomagnesemia
Many side effects of tacrolimus are similar to cyclosporine A, but tacrolimus does not cause gingival hyperplasia or hypertrichosis.
Both calcineurin inhibitors (cyclosporine A and tacrolimus) are highly nephrotoxic. They become even more nephrotoxic when combined and should, therefore, never be administered concurrently!
Purine analogs (azathioprine, mercaptopurine) [8]
- Pancytopenia; (leukopenia, macrocytic anemia, thrombocytopenia): exacerbated by interaction with allopurinol, since it inhibits xanthine oxidase, which is responsible for the degradation of 6-mercaptopurine
- Hepatotoxicity
- Malignancies, including cervical cancer, lymphoma, squamous cell carcinoma, melanoma (rare)
- Nausea, vomiting, and dose-related diarrhea
- Acute pancreatitis
To remember that Azathioprine is the precursor of 6-mercaptopurine, think “Azathiopurine.”
Allopurinol causes toxic accumulation of azathioprine! In cases in which concomitant treatment is unavoidable, a dose reduction of azathioprine is necessary!
mTOR inhibitors (sirolimus, everolimus) [9][10]
- Pancytopenia
- Insulin resistance
- Hyperlipidemia
- No nephrotoxicity
- Infection (e.g., respiratory or urinary tract)
- Peripheral edema
- Hypertension
- Stomatitis
To remember that sirolimus can cause pancytopenia, think “Sir, don't forget your pants!”
In contrast to calcineurin inhibitors, mTOR inhibitors are not nephrotoxic.
Mycophenolate mofetil [11]
- Pancytopenia
- Infection; (e.g., respiratory or urinary tract), especially with CMV
- Vomiting and diarrhea
- Hyperglycemia
- Hypertension
- Comparatively low neurotoxicity and nephrotoxicity
- Peripheral edema
- ↑ Blood urea nitrogen
- Hypercholesterolemia
- Back pain
- Cough
Methotrexate [3]
- Bone marrow suppression: pancytopeniaand/or macrocytic anemia
- Mucositis (particularly stomatitis, enteritis), susceptibility to infection
- Hepatotoxicity
- Nephrotoxicity
- Gastrointestinal side effects (e.g., nausea and vomiting)
- Diarrhea
- Pulmonary fibrosis and toxicity
- Rash
- Hair loss
- Increased risk of lymphoproliferative disorders
- Teratogenicity
Leucovorin salvage therapy [12]
- The side effects of methotrexate can be reduced by administering salvage therapy.
- Salvage therapy involves the administration of folic acid and folinic acid (active folic acid = leucovorin = calcium folinate).
- Indications
- Methotrexate (MTX) intoxication (inadvertent overdosage or impaired elimination): administered every 6 hours until methotrexate level < 10 mol
- Prophylactic therapy: within 24–48 h of starting high dose MTX
Biologics (e.g., daclizumab) [13]
-
General side effects
- Rash, dermatitis
- Formation of anti-drugantibodies (especially for adalimumab and infliximab): can manifest with a decrease in clinical response (e.g., recurrence of symptoms), low drug levels, and/or allergic reactions.
- Flu-like symptoms
- ↑ ALT, ↑ AST
- Lymphadenopathy
- Infections (e.g., nasopharyngitis)
- Gastrointestinal symptoms (e.g., diarrhea)
- Leukocytosis or leukopenia, thrombocytopenia, anemia
- Depression
- Rituximab and natalizumab: reactivation of a latent JC virus infection, resulting in progressive multifocal leukoencephalopathy (PML)
-
Basiliximab
- Tremor, shaking
- Hypertension
- Edema
- Allergic reaction
- Nausea, vomiting
- Cetuximab and panitumumab: : general side effects (especially rash, diarrhea, ↑ ALT, ↑ AST)
-
Bevacizumab
- Gastrointestinal perforation
- Hemorrhages (e.g., GI bleeding)
- Wound healing complications
- Thrombosis
- Trastuzumab: dilated cardiomyopathy (reversible in most cases)
-
TNF-α inhibitors
- Infections
- Reactivation of prior infections (e.g., latent TB)
- Drug-induced lupus
- Alemtuzumab: ↑ risk of developing autoimmune conditions (e.g., ITP) and infections
-
Nivolumab, pembrolizumab, and cemiplimab: ↑ risk of developing autoimmune conditions, including:
- Endocrinopathies
- Pneumonitis
- Dermatitis
- Enterocolitis
- Hepatitis
- Avelumab, durvalumab, and atezolizumab: same as above
- Ipilimumab: same as above
Before initiating anti-TNF-α treatment, a test for latent tuberculosis should be performed.
To remember that trastuzumab causes dilated cardiomyopathy, think “If you trust trustuzumab, it might break your heart.”
Contraindications to anti-TNF-α treatment (infliximab, adalimumab, etanercept)
- Pregnancy
- Chronic infections, particularly tuberculosis: Rule out latent tuberculosis before starting therapy (the activity of TNF-α plays a major role in formation and stabilization of granulomas against Mycobacterium tuberculosis).
- Multiple sclerosis
- Malignancy
- Immunosuppressed individuals
- Systemic or localized infections
- Moderate to severe heart failure (NYHA class III/IV)
Glucocorticoids
- For side effects of glucocorticoids see “Side effects of glucocorticoid therapy.”
We list the most important adverse effects. The selection is not exhaustive.