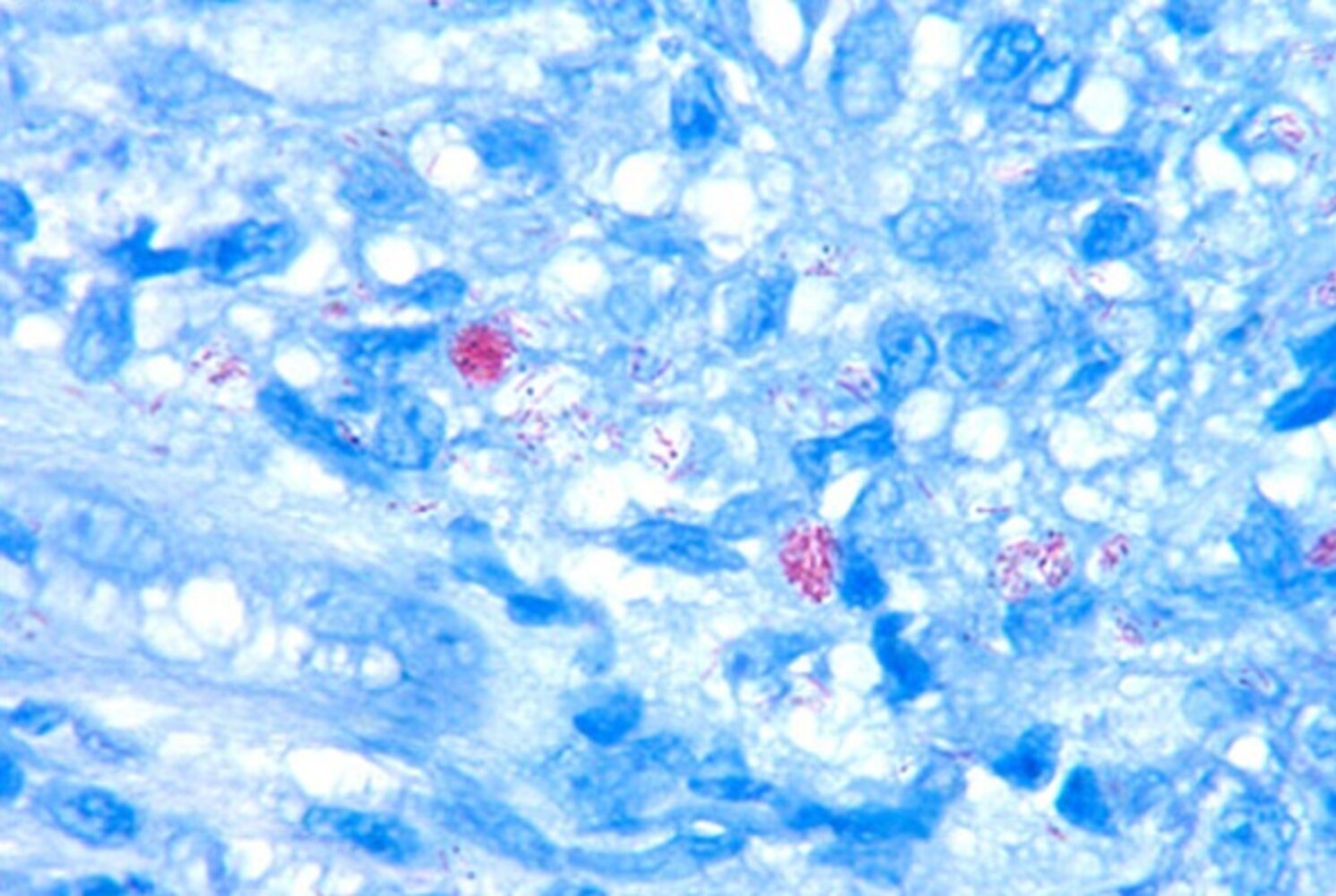
Leprosy (Hansen disease) is a chronic infectious disease caused by prolonged exposure to Mycobacterium leprae, an acid-fast, slow-growing, fastidious bacillus. Leprosy primarily occurs in tropical and/or developing countries and is rarely observed in the US. There are various forms whose descriptions differ among two different classification systems, but the three cardinal clinical manifestations of leprosy are hypopigmented skin lesions, nerve thickening, and peripheral nerve palsies. Long-standing cases of leprosy classically develop deformities as a result of contractures following motor nerve palsies and/or repeated injury due to sensory loss. Other chronic complications include uveitis, orchitis, and nasal septal perforation. Patients with leprosy may also present with acute lepra reactions that are characterized by painful skin lesions and neuritis. The diagnosis is usually confirmed with the help of a biopsy. Lepromin tests aid in the classification of various forms of leprosy. Treatment consists of prolonged MDT (multi-drug therapy) with dapsone and rifampin. Clofazimine is added to the therapeutic regimen in patients with multibacillary leprosy.
- Incidence: ∼ 150 new cases annually [1]
- Prevalence: ∼ 0.2/10,000 worldwide [2]
- Peak incidence: 10–15 and 30–65 years [3]
- Sex: ♂ > ♀ [4]
- Endemic to tropical regions: India, Brazil, Indonesia, Nepal, Myanmar, Nigeria
Epidemiological data refers to the US, unless otherwise specified.
- Pathogen: Mycobacterium leprae is an obligate, intracellular, acid-fast bacillus that cannot be cultured and thrives in cold temperatures. [5]
-
Route of transmission
- Close contact with fomites, contaminated soil, infected individuals, and nine-banded armadillos (in rare cases)
- Respiratory droplet transmission
- Risk factors are close contact with infected individuals or contaminated soil.
- Although transmission is rare, infected animals (e.g., armadillos, mangabey monkeys, sphagnum moss) pose a potential risk in the US.
- Transmission usually requires prolonged exposure, and some individuals seem more predisposed than others.
- Infectious type: lepromatous leprosy (see “Pathophysiology” below)
- Reservoirs: infected humans; , nine-bandedarmadillos in the US
| Pathophysiology of lepromatous and tuberculoid leprosy [6] | |||||
|---|---|---|---|---|---|
| Lepromatous leprosy (LL) | Tuberculoid leprosy (TT) | ||||
| Characteristics |
|
|
|||
Leprosy is a slowly progressive, chronic infection with a spectrum of clinical manifestations depending on the degree of cell-mediated immunity.
- Incubation period: 3–5 years
- The clinical manifestations vary depending on the type of leprosy (LL, TT, or several intermediate forms collectively known as borderline leprosy.
| Clinical features of lepromatous and tuberculoid leprosy [8] | |||||
|---|---|---|---|---|---|
| Lepromatous leprosy (LL) | Tuberculoid leprosy (TT) | ||||
| Cutaneous manifestations |
|
|
|||
| Nerve involvement |
|
|
|||
| |||||
| Systemic manifestations |
|
|
|||
The three cardinal clinical manifestations of leprosy are hypopigmented skin lesions, nerve thickening, and peripheral nerve palsies.
All peripheral nerves can become affected in leprosy, but the most commonly affected are the ulnar and the peroneal nerves.
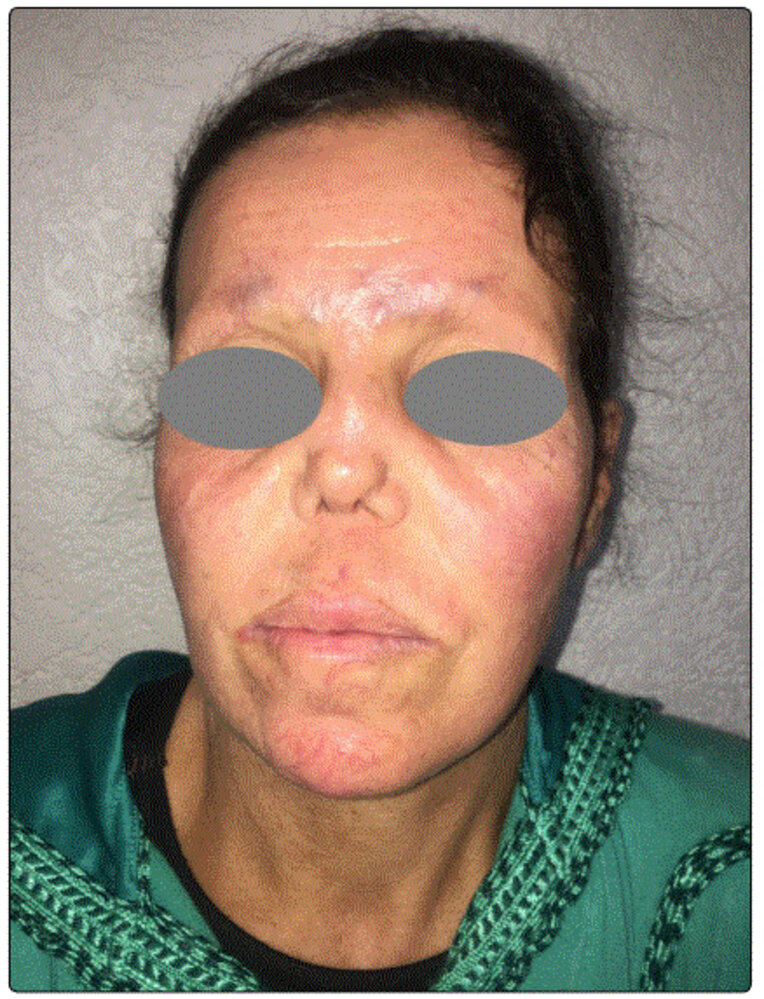
Lepromatous leprosy manifests with Leonine facies. The Low cell-mediated immunity in this condition makes it more Lethal (more communicable).



| Diagnostic characteristics of lepromatous and tuberculoid leprosy | |||
|---|---|---|---|
| Diagnostic test | Test characteristics | Lepromatous leprosy (LL) | Tuberculoid leprosy (TT) |
| Skin scraping or slit-skin smear |
|
|
|
| Punch biopsy |
|
|
|
| Lepromin test [12] |
|
|
|
Diffuse hypergammaglobulinemia associated with lepromatous leprosy can cause false-positive VDRL, RF, and/or ANA tests and thus result in diagnostic confusion.
Definitive therapy [13]
| Multidrug treatment of leprosy | |||
|---|---|---|---|
| Drugs | Lepromatous leprosy (LL) | Tuberculoid leprosy (TT) | |
| Dapsone | Yes | Yes | |
| Rifampin | Yes | Yes | |
| Clofazimine | Yes | No | |
Supportive therapy [6]
- Treatment of leprosy reactions (see “Complications” below)
-
Rehabilitation
- Physiotherapy to prevent contractures
- Surgery to correct deformities (e.g., tendon transfer surgery for ulnar nerve palsy)
- Wound care
-
Secondary deformities
- Bone destruction → shortened digits, autoamputation
- Neuropathic ulcers on the dorsum of the foot
- Charcot joints
-
Nasal complications
- Saddle nose deformity
- Anosmia
- Nasal septum perforation
-
Ocular complications
- Lagophthalmos and corneal insensitivity → corneal ulcers
- Invasion of the anterior chamber → chronic uveitis → blindness
-
Other complications
- Orchitis → testicular atrophy → hypergonadotropic hypogonadism
- Reactive amyloidosis
- Leprosy reactions
| Leprosy reactions | |||
|---|---|---|---|
| Type of lepra reaction | Type 1 (reversal reaction) [14] | Type 2 (erythema nodosum leprosum, ENL) [15][16] | Lucio phenomenon [17][18] |
| Mechanism |
|
|
|
| Cutaneous lesions |
|
|
|
| Neuritis |
|
|
|
| Systemic manifestations |
|
|
|
| Treatment |
|
|
|
Treatment of leprosy should not be stopped when leprosy reactions occur.
The presence of tender nerves in a patient with leprosy indicates a leprosy reaction.
We list the most important complications. The selection is not exhaustive.