Lipid disorders encompass a spectrum of metabolic conditions that affect blood lipid levels. They are generally characterized by elevated levels of cholesterol, triglycerides, and/or lipoproteins in the blood, which are often associated with atherosclerotic cardiovascular disease (ASCVD). Hyperlipidemia is most commonly a result of genetic predisposition in combination with lifestyle factors (e.g., diet, lack of activity, alcohol consumption). Hyperlipidemia resulting from single-gene disorders, e.g., familial hypercholesterolemia, can cause severe elevations in lipoprotein levels and early atherosclerotic complications. Lipid disorders are usually detected during laboratory testing as part of an ASCVD risk assessment. A serum lipid panel includes total cholesterol, LDL, HDL, and triglyceride levels. Lipid-lowering therapy is indicated to reduce the risk of cardiovascular disease in adults with LDL > 190 mg/dL, diabetes mellitus, and established ASCVD, and should be considered for other patients based on individual ASCVD risk. The main treatment modalities are lifestyle modifications and lipid-lowering agents such as statins. For individuals < 20 years, see “Pediatric dyslipidemia” for information on screening, diagnostic cut-offs, and management.
Abetalipoproteinemia is a congenital lipid disorder in which a deficiency of apolipoproteins (hypolipoproteinemia) leads to impaired intestinal absorption of fats and fat-soluble vitamins. Symptoms usually appear during childhood and mainly consist of failure to thrive, steatorrhea, and signs of vitamin E deficiency. Treatment includes vitamin E supplementation.
- Dyslipidemia: an abnormal concentration of lipids in the blood (e.g., high or low LDL cholesterol)
-
Hyperlipidemia: elevated blood lipid levels (e.g., total cholesterol, LDL cholesterol, and/or triglycerides)
- Hypercholesterolemia: elevated cholesterol levels (most commonly measured with LDL) based on age and ASCVD risk factors
- Hyperlipoproteinemia: elevated levels of serum lipoproteins (e.g., high VLDL)
- Hypertriglyceridemia: elevated triglyceride levels (e.g., > 150 mg/dL in adults)
-
Prevalence of hypercholesterolemia
- Elevated total cholesterol levels: ∼ 38% [1]
- Elevated LDL cholesterol levels: ∼ 29% [1]
- Prevalence of hypertriglyceridemia: ∼ 26% [1]
Epidemiological data refers to the US, unless otherwise specified.
- Usually multifactorial [2]
- Secondary causes of dyslipidemia
- Genetic causes
- Polygenic disease is common, e.g., polygenic type II dyslipidemia. [3]
- Monogenic disease is less common, e.g., heterozygous familial type IIa dyslipidemia (1:200–500 people). [3]
- See also “Frederickson classification of monogenic hyperlipidemias.”
Severe dyslipidemia (e.g., LDL > 190 mg/dL) suggests an underlying monogenic disorder and/or a strong polygenic predisposition. [2]
| Secondary causes of dyslipidemia [2][4][5] | ||
|---|---|---|
| Elevated LDL cholesterol | Elevated triglycerides | |
| Lifestyle factors |
|
|
| ||
| Drugs |
|
|
| ||
| Medical conditions |
|
|
| ||
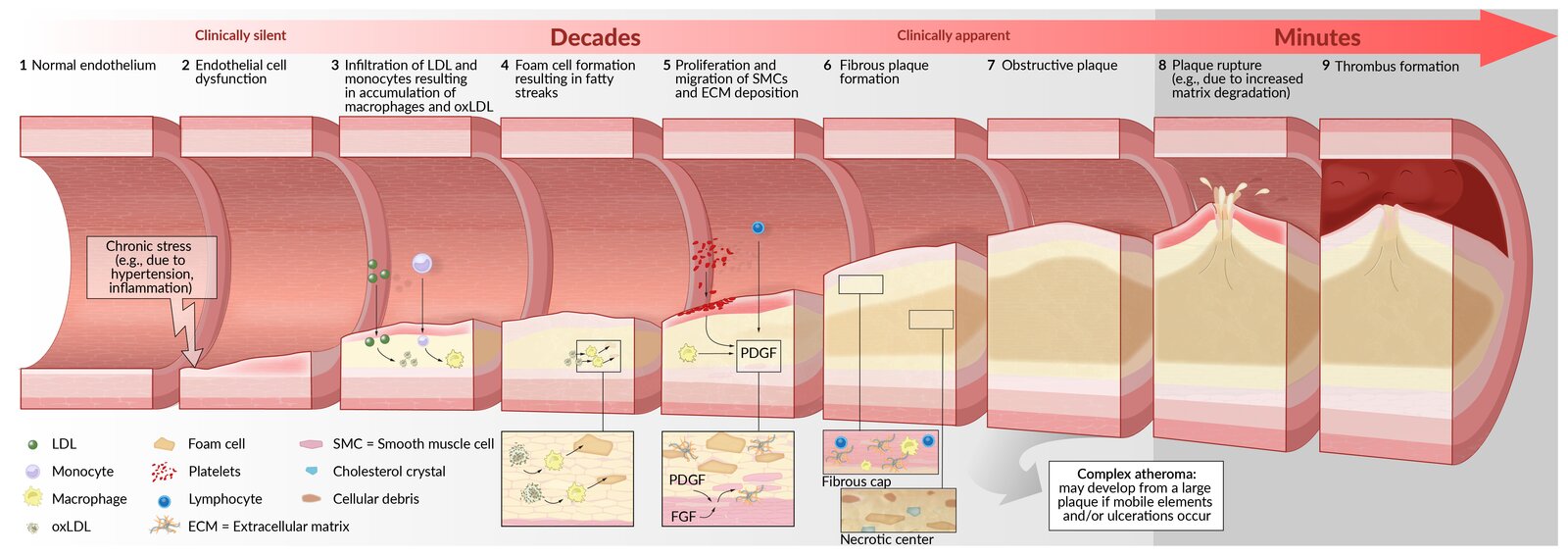
- Elevated LDL cholesterol and reduced HDL cholesterol promote atherosclerosis → increased risk of cardiovascular events
- See “Pathogenesis of atherosclerosis.”
Dyslipidemia is a major risk factor for ASCVD.
- Dyslipidemia is usually asymptomatic.
- Severe and/or persistent elevation can cause:
- Benign skin and/or eye manifestations, e.g., xanthelasma, lipemia retinalis
- Complications, e.g., atherosclerosis, hepatic steatosis
- In genetic lipid disorders, symptoms generally occur at an earlier age and are more severe than in acquired lipid disorders.
Skin manifestations
Xanthomas
- Description: nodular lipid deposits in the skin and tendons
- Pathophysiology: : Extremely high levels of triglycerides and/or LDL cholesterol result in extravasation of plasma lipoproteins and their deposition in tissue.
- Histology: large perivascular infiltrates with foam cells (lipid-ladenmacrophages) and multinucleated histiocytes called Touton giant cells
| Types of xanthomas | |||
|---|---|---|---|
| Description | Location | Associated condition | |
| Eruptive xanthoma |
|
|
|
| Tuberous xanthoma |
|
|
|
| Tendinous xanthoma |
|
|
|
| Palmar xanthoma |
|
|
|
| Plane xanthoma |
|
|
|
:
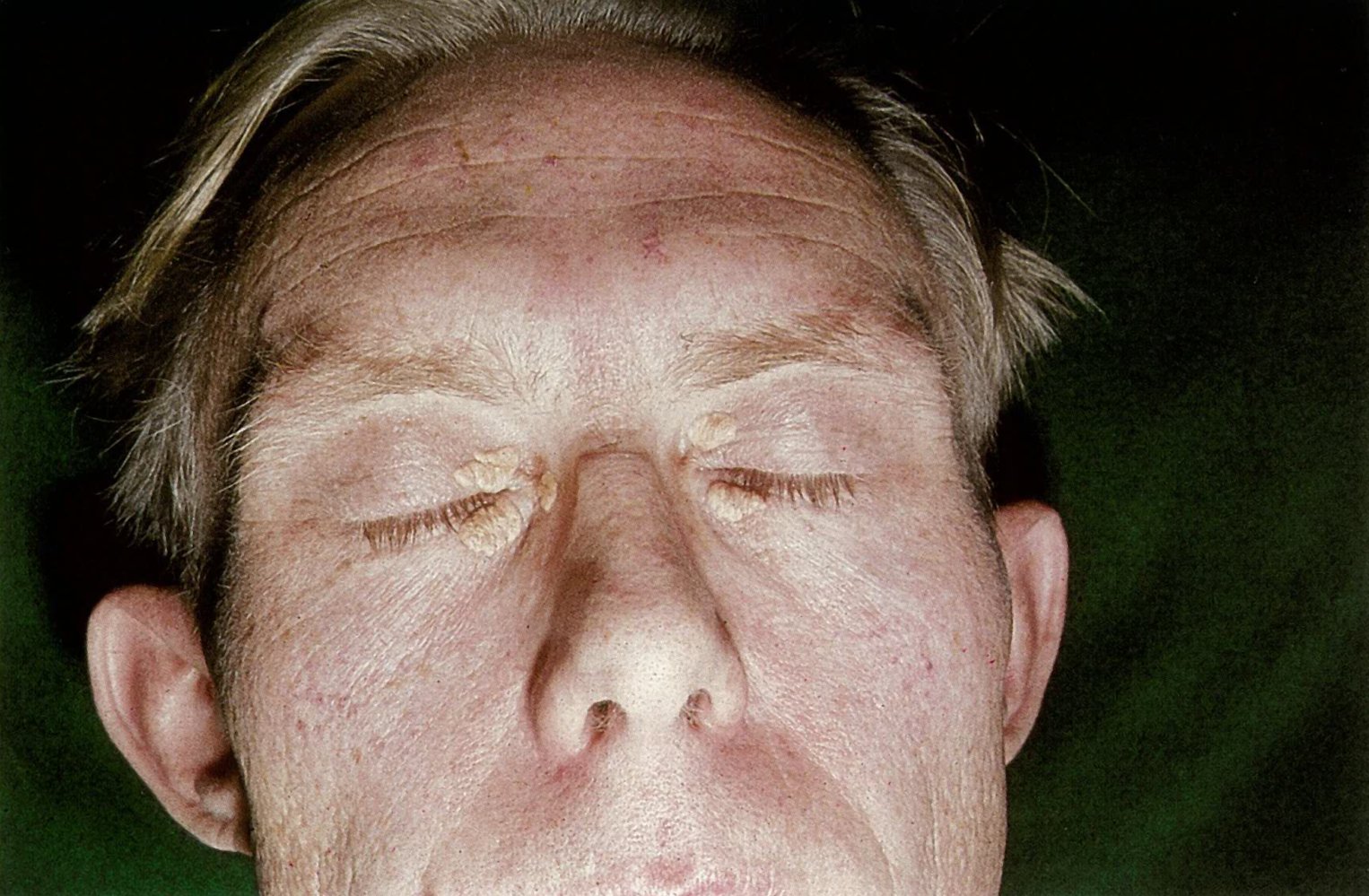
Xanthelasmas
- Description: typically bilateral, yellow, flat plaques on the upper eyelids (nasal side)
-
Etiology
- Idiopathic
- Increased incidence in:
- Patients with diabetes mellitus
- Patients with increased lipoproteins in plasma
- Usually affects postmenopausal women
- Associated conditions: hypercholesterolemia (e.g., primary biliary cholangitis), hyperapobetalipoproteinemia, ↑ LDL cholesterol levels


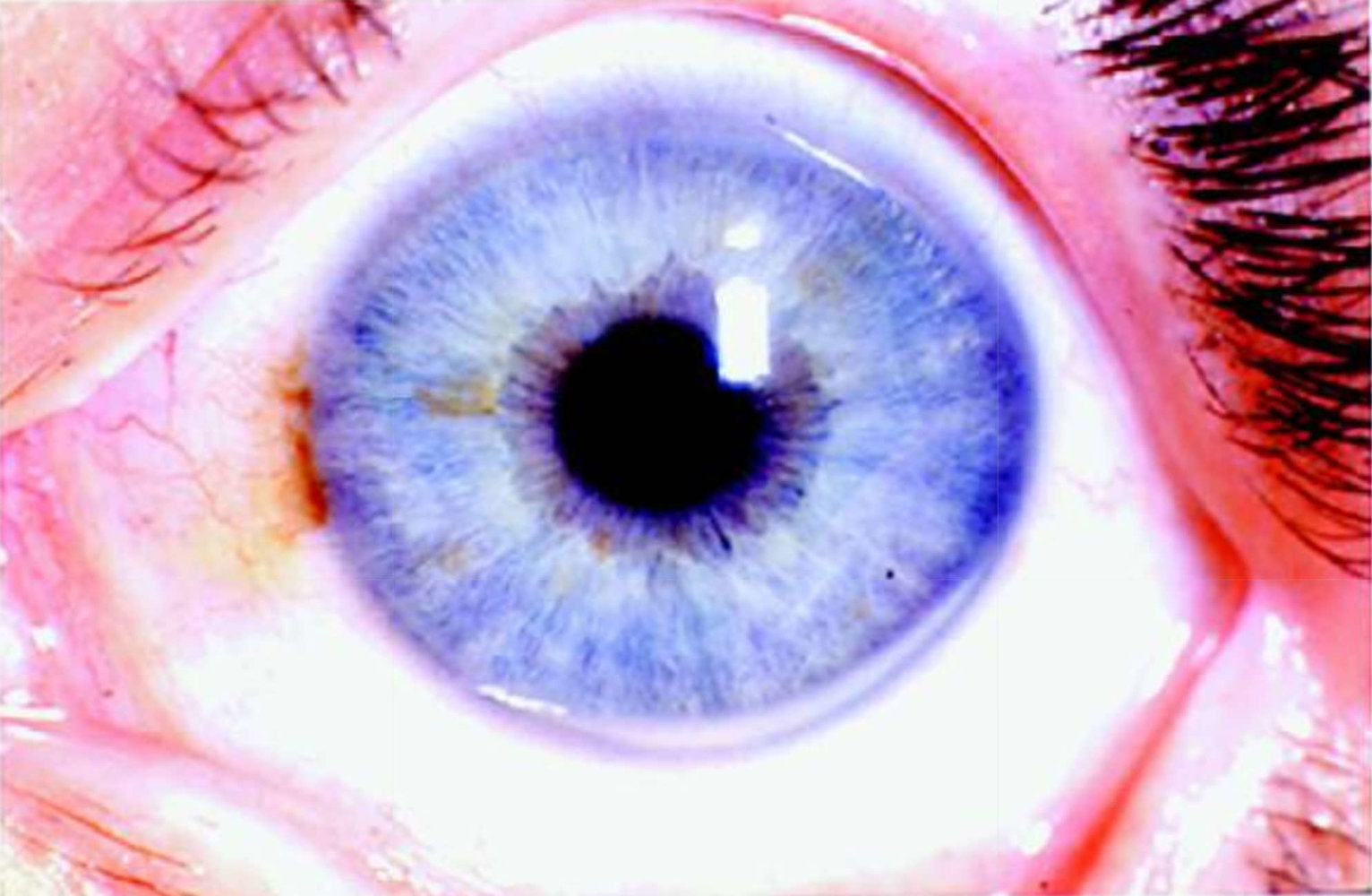
Eye manifestations
-
Lipemia retinalis
- Description: opaque, white appearance of the retinal vessels, visible on fundoscopic exam
- Associated condition: hyperlipoproteinemia type I, III, and IV
-
Arcus lipoides corneae
- Associated with hyperlipoproteinemia type II
- Not pathological in advanced age
Overview of inherited hyperlipoproteinemia
This table describes monogenic dyslipidemias; polygenic dyslipidemia can also be categorized based on disease phenotype using the Frederickson classification. [3]
| Frederickson classification of monogenic hyperlipoproteinemia [9] | ||||||
|---|---|---|---|---|---|---|
| I | Type II hyperlipoproteinemia | III | Type IV hyperlipoproteinemia | V | ||
| IIa | IIb | |||||
| Condition |
|
|
|
|
|
|
| Frequency [3] |
|
|
|
|
|
|
| Inheritance |
|
|
|
|
|
|
| Pathogenesis |
|
|
|
|
|
|
| Clinical manifestations |
|
|
|
|
|
|
| Lipoprotein defect |
|
|
|
|
|
|
| Total cholesterol |
|
|
|
|
|
|
| Elevated serum lipoproteins |
|
|
|
|
|
|
| Total triglycerides |
|
|
|
|
|
|
| Overnight plasma |
|
|
|
|
|
|
Abetalipoproteinemia
-
Etiology
- Deficiency of apolipoproteins (ApoB-48, ApoB-100)
- Due to a mutation in the microsomal triglyceride transfer protein (MTTP) gene
-
Pathophysiology
- Autosomal recessive disease
- Deficiency of chylomicrons, VLDL, and LDL (hypolipoproteinemia)
-
Clinical features
-
Early
- Steatorrhea
- Failure to thrive
- Fat malabsorption → fat-soluble vitamin deficiency
- Acanthocytosis
-
Late
- Developmental delay
- Retinitis pigmentosa
- Myopathy
- Progressive ataxia
- Spinocerebellar degeneration as a result of vitamin E deficiency
-
Early
-
Diagnostics
- Extremely low levels of plasma cholesterol (< 50 mg/dL)
- Acanthocytes in the blood
- Other tests performed include complete blood count with differential, stool studies, and fasting lipid profile.
- Confirmatory test: genetic testing to detect mutations in the MTTP gene
- Intestinal biopsy: Histology may reveal lipid-laden enterocytes.
-
Treatment
- Vitamin E supplementation (high doses)
- Reduced long-chain fatty acids intake
Chylomicronemia syndrome [16]
- Definition: a constellation of symptoms resulting from severely elevated serum triglyceride levels (> 1500 mg/dL) [16]
-
Etiology
- Genetic causes (e.g., familial hypertriglyceridemia, familial partial lipodystrophy)
- Multifactorial chylomicronemia syndrome (MFCS)
-
Clinical features
- Abdominal pain
- Eruptive xanthomas
- Lipemia retinalis
- Confusion and memory loss
- Diagnostics: fasting serum triglyceride level
-
Management
- A very low-fat diet until triglyceride levels are < 1000 mg/dL. [16]
- Mitigate secondary causes of hyperlipidemia.
- If triglyceride levels remain > 500 mg/dL: [16]
- Initiate fibrates.
- If still elevated after fibrates, add omega-3 fatty acids and/or niacin.
- Initiate ASCVD prevention once triglyceride levels are < 500 mg/dL. [16]
-
Complications
- Acute pancreatitis
- ASCVD
A very low-fat diet is the mainstay of therapy for patients with familial hyperchylomicronemia, as there is typically minimal response to lipid-lowering medications. [16]
General principles [17][18]
- Order a lipid panel when evaluating patients with a known secondary cause of dyslipidemia, e.g., diabetes mellitus or nephrotic syndrome.
- Screen for lipid disorders based on age and family history.
- If lipid levels are abnormal:
- Repeat a lipid panel at least once to confirm the diagnosis. [2]
- Assess for secondary causes of dyslipidemia. [1]
- Calculate ASCVD risk.
- Consider testing for monogenic disorders based on clinical suspicion. [17]
Screening for lipid disorders [1]
-
Adults age 20–75 years: A nonfasting or fasting lipid panel (FLP) is acceptable. [17]
- Screen at least every 4–6 years. [19]
- See “ASCVD risk assessment" for details.
- Individuals < 20 years: See “Pediatric dyslipidemia screening.”
Diagnostic confirmation [5][17][18]
For individuals < 20 years, see “Diagnostics for pediatric dyslipidemia” for different cut-off values.
-
Lipid panel: includes total cholesterol, HDL, LDL, and triglycerides
- Nonfasting is appropriate for most situations.
- Fasting lipid panel is indicated if initial triglycerides are ≥ 400 mg/dL.
- Other tests
- Direct measurement of LDL cholesterol: indicated if the estimated level is < 70/mg/dL [17][20]
- Lipoprotein(a) and apolipoprotein B: Consider as part of ASCVD risk assessment. [17][18]
Normal lipid levels
For individuals < 20 years, see “Diagnostics for pediatric dyslipidemia” for different cut-off values.
- Total cholesterol: < 200 mg/dL
- HDL cholesterol: ≥ 40 mg/dL for men; ≥ 50 mg/dL for women [21]
- Non-HDL cholesterol < 130 mg/dL [22]
-
LDL cholesterol: depends on ASCVD risk [18]
- < 100 mg/dL in adults at average risk
- < 70 mg/dL in patients with ASCVD or at high risk
- Triglycerides: < 150 mg/dL
- Lipoprotein(a): < 50 mg/dL
- Apolipoprotein B: < 130 mg/dL
Assays for apolipoprotein B and lipoprotein(a) are not formally standardized and results may therefore be unreliable.
Additional evaluation [1][2][18]
Secondary causes [1][2][18]
- Obtain the following studies based on clinical suspicion.
- Fasting blood glucose or HbA1c [23][24]
- TSH
- Liver chemistries to screen for cholestatic liver disease [1]
- Urinalysis and serum creatinine to screen for renal disease, e.g., nephrotic syndrome
- HIV testing [18]
- Testing for autoimmune diseases, e.g., SLE diagnostics
- Consider other secondary causes based on patient history, e.g., antipsychotic use or lifestyle factors
Monogenic causes [2][5][25][26]
- Clinical scoring systems (e.g., Dutch Lipid Clinic Network criteria) may be used to diagnose familial hypercholesterolemia.
- Refer for targeted gene sequencing if results will influence management decisions. [2]
- Factors that increase suspicion for a monogenic disorder include: [2][25]
- Persistent and/or severe dyslipidemia, e.g., LDL cholesterol > 190 mg/dL
- Premature ASCVD [26]
- Family history of premature ASCVD or dyslipidemia
- Concerning clinical features, e.g., achilles tendon xanthoma [2]
This section focuses on the treatment of severe LDL cholesterol and triglyceride elevations in adults. For adults with nonsevere hyperlipidemia, the calculated ASCVD risk determines treatment. . For children, see “Management of pediatric dyslipidemia.”
Approach [1][17]
-
Encourage lifestyle modifications for ASCVD prevention for all patients, including:
- Physical activity
- Dietary modifications
- Mitigate secondary causes of hyperlipidemia.
- Limit alcohol use.
- Manage associated medical conditions (e.g., diabetes mellitus).
- Avoid medications that increase triglyceride or cholesterol levels.
- Initiate pharmacotherapy based on the type and severity of dyslipidemia.
- Consult a lipid specialist for patients with:
- Inherited hyperlipoproteinemias
- Statin intolerance
- Persistent hypercholesterolemia (e.g., for treatment with LDL apheresis) [17]
Unaddressed secondary causes of dyslipidemia can prevent patients from responding to treatment for monogenic disease (e.g., familial hyperlipidemia). [2]
Pharmacotherapy
Very high LDL cholesterol [17][26][27]
- Indication: LDL cholesterol ≥ 190 mg/dL in adults 20–75 years of age [17]
-
Goals
- ≥ 50% reduction in LDL cholesterol levels from baseline (with maximally tolerated statin therapy)
-
LDL cholesterol targets vary, e.g.:
- 20–75 years of age (regardless of etiology or ASCVD risk): < 100 mg/dL [17]
- 30–75 years of age with heterozygous familial hypercholesterolemia and established ASCVD: < 70 mg/dL [28][29]
- First-line treatment: high-intensity statin therapy, e.g., atorvastatin or rosuvastatin [17]
-
Subsequent treatment
- Repeat lipid panel 6–12 weeks after treatment initiation or dose adjustment. [2][5]
-
If treatment goals are not met, consider adding nonstatin lipid-lowering agents sequentially, e.g.:
- Ezetimibe [17]
- PCSK9 inhibitor, e.g., evolocumab or alirocumab
- Bile acid sequestrant, e.g., colesevelam
- Lomitapide (in patients with homozygous familial hypercholesterolemia)
Severe hypertriglyceridemia [1][6][17]
For children, see “Management of pediatric dyslipidemia.”
- Indication: fastingtriglycerides> 500 mg/dL
-
First-line treatment
- Fibrates, e.g., fenofibrate or gemfibrozil
- OR omega-3 fatty acids, e.g., icosapent ethyl or omega-3-acid ethyl esters
-
Subsequent treatment if triglycerides remain > 500 mg/dL [1]
- Fibrates PLUS omega-3 fatty acids (recommended)
- Consider adding niacin. [5]
Treatment with statins may still be indicated in patients with LDL cholesterol < 190 mg/dL and/or triglycerides < 500 mg/dL, depending on ASCVD risk.
Xanthoma and xanthelasma [30][31]
- Treatment may be considered for cosmetic reasons, but recurrence is common.
- Methods include surgical, laser, and/or topical therapy.
- Hepatic steatosis: associated with abetalipoproteinemia
-
Hypertriglyceridemia-induced pancreatitis
- May occur in severe hypertriglyceridemia (typically > 1,000 mg/dL)
- Associated conditions include hyperlipoproteinemia types I and IV.
-
ASCVD
-
Manifests with secondary diseases, e.g.:
- Coronary heart disease
- Myocardial infarction
- Stroke
- Peripheral arterial disease
- Carotid artery stenosis
- Cholesterol embolization syndrome
- Hyperlipoproteinemia types II, III; , and IV are associated with premature atherosclerosis.
-
Manifests with secondary diseases, e.g.:
Triglyceride levels ≥ 500 mg/dL increase the risk of pancreatitis. [32]
We list the most important complications. The selection is not exhaustive.
- One-Minute Telegram 123-2025-2/3: A single injection of lepodisiran provides long-term lipoprotein(a) reduction
- One-Minute Telegram 71-2023-2/3: Statin your case: high-intensity therapy vs. treat-to-target for elevated LDL cholesterol
Interested in the newest medical research, distilled down to just one minute? Sign up for the One-Minute Telegram in “Tips and links” below.