Metabolic syndrome is the co-occurrence of medical conditions that increase the risk for atherosclerotic cardiovascular disease (ASCVD) and type 2 diabetes: elevated blood glucose, hypertension, dyslipidemia, and/or abdominal obesity. Management of metabolic syndrome includes optimization of cardiovascular health (e.g., lifestyle modifications for ASCVD prevention) and treatment of the individual components of metabolic syndrome (e.g., management of hypertension and treatment of hyperlipidemia). Screening for the individual components of metabolic syndrome is recommended; the frequency and nature of screening varies based on risk factors. Cardiovascular-kidney-metabolic (CKM) syndrome is an emerging concept developed by the American Heart Association to describe the interaction between metabolic risk factors (e.g., obesity, diabetes, hypertension, hypertriglyceridemia), chronic kidney disease (CKD), and cardiovascular disease (CVD). Adverse social determinants of health (SDOH) are known to increase the risk for both metabolic syndrome and CKM syndrome and should be addressed as part of management.
The prevalence of metabolic syndrome is increased in: [1]
- Individuals with certain adverse SDOH (e.g., lower income families)
- Older adults compared to younger adults
Epidemiological data refers to the US, unless otherwise specified.
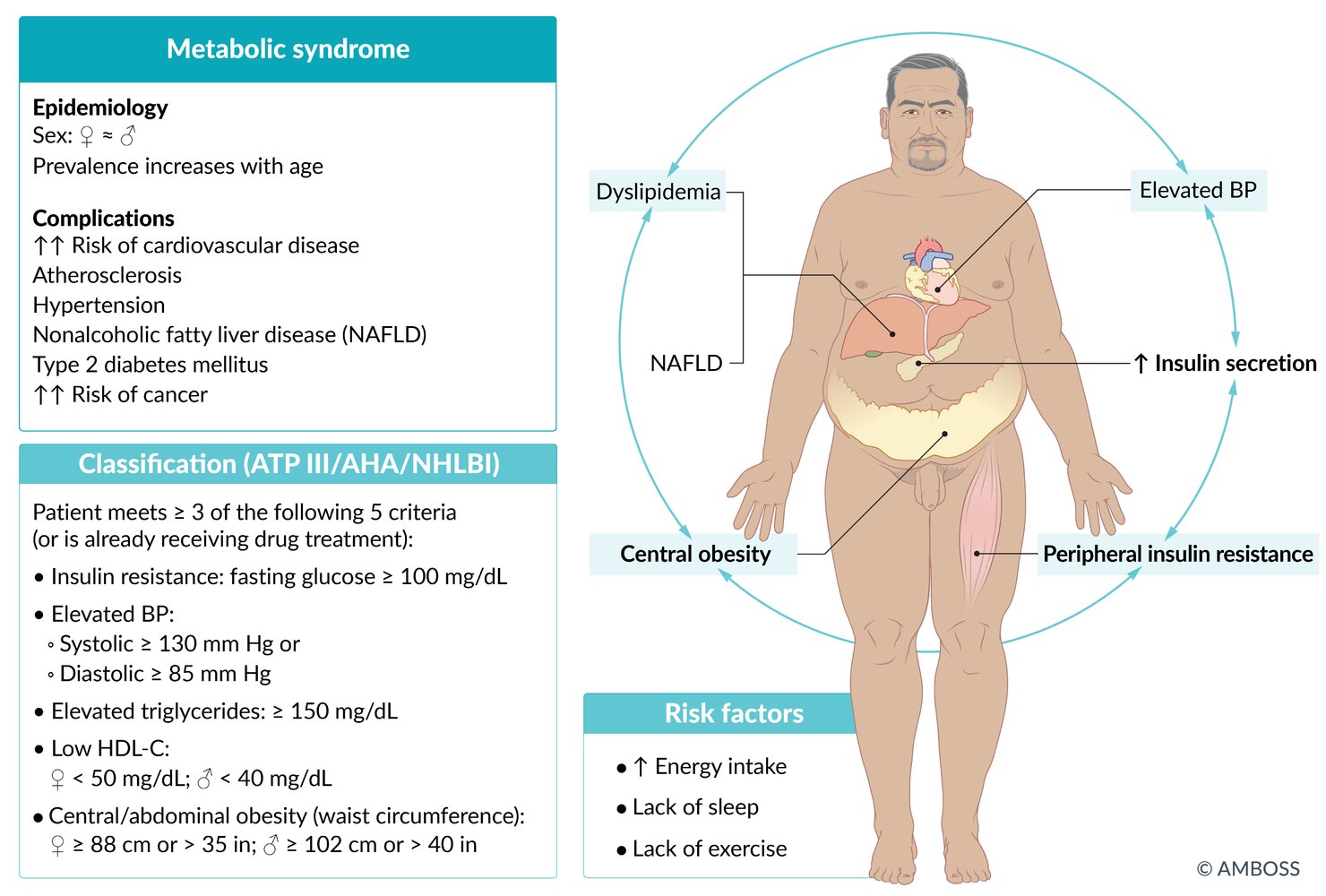
Dysfunctional adipose tissue → inflammation and insulin resistance → abnormal lipid and glucose metabolism [2]
Abdominal obesity (i.e., accumulation of fat in visceral tissue) is strongly associated with an atherogenic and hyperglycemic state. [2][3]
Metabolic syndrome is diagnosed in patients with or receiving treatment for ≥ 3 of the following conditions: [2][3][4]
-
Abdominal obesity
- Most populations in the US [5][6]
- Men: waist circumference≥ 102 cm (40 in)
- Women: waist circumference≥ 88 cm (35 in)
- People of Asian descent [6][7]
- Men: waist circumference ≥ 90 cm (35.4 in)
- Women: waist circumference ≥ 80 cm (31.5 in)
- Most populations in the US [5][6]
- Elevated triglycerides: ≥ 150 mg/dL (or receiving drug treatment for elevated triglycerides)
-
Low HDL-C (or receiving drug treatment for reduced HDL)
- Men: < 40 mg/dL
- Women: < 50 mg/dL
- Elevated blood pressure: systolic ≥ 130 mm Hg and/or diastolic≥ 85 mm Hg (or receiving drug treatment for hypertension)
- Elevated blood glucose: fasting glucose ≥ 100 mg/dL (or receiving drug treatment for elevated glucose)
- Manage individual components of metabolic syndrome, e.g.: [2][3]
- Treatment of obesity
- Management of hypertension
- Treatment of hyperlipidemia
- Treatment of diabetes
- Optimize cardiovascular health, e.g., by: [2][3]
- Educating on Life's Essential 8 [8]
- Recommending lifestyle modifications for ASCVD prevention
- Screening for and treating other components of CKM syndrome
- Manage associated conditions, e.g.: [2][3]
- Management of obstructive sleep apnea
- Treatment of polycystic ovary syndrome
Management of metabolic syndrome may require a multidisciplinary approach; refer to specialists (e.g., endocrinology, cardiology, obesity medicine) as needed.
Primary prevention
See “Primary prevention of ASCVD.”
Screening for components of metabolic syndrome [2][8]
-
BMI and waist circumference
- Measure annually, typically at routine health maintenance visits
- See “BMI classification for overweight and obesity” for details.
- Dyslipidemia: See “Screening for lipid disorders” and “Pediatric dyslipidemia screening.”
- Hypertension: See “Screening for hypertension” and “Screening for hypertension in children.”
- Elevated blood glucose: See “Screening for diabetes mellitus.”
- See also “Screening for CKM syndrome.”
Cardiovascular-kidney-metabolic (CKM) syndrome is an emerging concept developed by the American Heart Association to describe the interaction between metabolic risk factors (e.g., obesity, diabetes, hypertension), CKD, and CVD, which can result in multiorgan dysfunction and poor cardiovascular outcomes. [8]
Pathophysiology
Biological and environmental risk factors and SDOH → dysfunctional adipose tissue → inflammation and insulin resistance → CKM risk factors (e.g., dyslipidemia, diabetes) and/or CKD → subclinical atherosclerosis, subclinical myocardial dysfunction, and/or progressive decline of renal function → poor health outcomes (e.g., stroke, heart failure, atrial fibrillation, coronary artery disease, ESRD) → disability and death [8]
CKM syndrome starts early in life and progresses over time. [8]
Screening for CKM syndrome
In addition to the factors listed below, screen children and adults routinely for SDOH.
Age < 21 years [8]
- Overweight and obesity: Screen annually using CDC growth charts for age and sex.
-
Hypertension: Start assessing at 3 years of age.
- No risk factors: Screen annually.
- Risk factors present: Screen at every health care visit.
-
Hypercholesterolemia
- Obtain a fasting lipid panel once between 9 and 11 years of age; start at 2 years of age in patients with additional risk factors.
- Repeat a fasting lipid panel once between 17 and 21 years of age.
-
Diabetes and MASLD [8]
- 9–11 years of age with overweight or obesity and risk factors for T2DM or risk factors for MASLD: Obtain hyperglycemia testing and ALT once.
- If results are normal, repeat every 2–3 years in patients with obesity, or who are overweight with one additional risk factor
-
Mental and behavioral health
- Screen at least annually for all children. See “Mental and social health screening” in "Well-child visits" for details.
Age ≥ 21 years [8]
-
Metabolic syndrome components
- BMI and waist circumference: Measure annually.
-
Blood pressure measurement, hyperglycemia tests, and lipid panel :
- CKM stage 0: obtain every 3–5 years
- CKM stage 1 (or history of gestational diabetes): obtain every 2–3 years
- CKM stage 2: obtain annually
- MASLD-related advanced fibrosis: Obtain a FIB-4 score every 1–2 years in individuals with diabetes, prediabetes, or ≥ 2 metabolic risk factors.
-
Kidney disease: UACR, serum creatinine, and serum cystatin C
- CKM stage 2 or higher: obtain annually
- Very high risk of progression of CKD: obtain more frequently according to current guidelines
-
ASCVD [9][10]
- See “ASCVD risk assessment” for details on screening frequency and tools, e.g., PREVENTTM equations.
- Consider coronary artery calcium score for patients with borderline or intermediate 10-year ASCVD risk.
-
Heart failure
- There is no strong recommendation for screening to detect preclinical heart failure.
- Consider echocardiogram and/or cardiac biomarkers on a case-by-case basis according to age, comorbidities, and ASCVD risk score.
Subsequent screening intervals are based on the CKM stage.
Staging [8]
Staging is based on the presence of CKM risk factors.
CKM risk factors
-
Excess and/or dysfunctional adiposity
- Overweight or obesity (elevated BMI)
- Abdominal obesity
- Prediabetes
-
Other metabolic CKM risk factors
- Type 2 diabetes
- Hypertension
- Hypertriglyceridemia ≥ 135 mg/dL
- Metabolic syndrome
Risk-enhancing factors
Risk-enhancing factors are elements that heighten the chances of advancing through stages of CKM syndrome and raise the risk of developing CVD and kidney failure. [8]
- ASCVD risk-enhancing factors
- Adverse SDOH (e.g., low socioeconomic status)
- Mental health disorders (e.g., anxiety and depression)
- Other sex-specific factors (e.g., early menopause, pregnancy complications, erectile dysfunction, PCOS)
CKM staging [8]
The CKM staging framework illustrates the interactions between CKM components and the risk of progression into clinical CVD with or without renal failure.
| CKM staging [8] | |||
|---|---|---|---|
| Stage | Definition | ||
| CKM stage 0 |
|
||
| CKM stage 1 |
|
||
| CKM stage 2 |
|
||
| CKM stage 3 |
|
||
| CKM stage 4 |
|
||
Management
- Promote overall health for patients with all stages of CKM syndrome, e.g.:
- Provide education about Life's Essential 8.
- Encourage lifestyle modifications for ASCVD prevention.
- Address relevant CKM syndrome components, e.g.:
- Management of ASCVD
- Management of heart failure
- Management of Afib
- Treatment of coronary artery disease
- Management of CKD
CKM stage 2 or higher should be managed by a multidisciplinary care team.