Peripheral edema is the accumulation of excess fluid in the tissues, particularly in the feet and legs. Although peripheral edema is often a manifestation of underlying systemic diseases, including heart failure, kidney disease (e.g., nephrotic syndrome), and cirrhosis, it can also result from localized issues such as chronic venous insufficiency or lymphatic obstruction and is a common side effect of some medications (e.g., calcium channel blockers). Peripheral edema manifests with swelling of the affected areas, which may be accompanied by skin tightness, discomfort, and, in severe cases, pain. Diagnosis involves a thorough patient history and physical examination, supported by laboratory tests and imaging studies to identify the underlying cause. Management strategies are primarily directed at treating the root cause of the edema, while symptoms can be relieved with limb elevation, compression therapy, and diuretics when fluid overload is a contributing factor.
Pulmonary edema, pleural effusion, ascites, angioedema, and cerebral edema are discussed in separate articles.
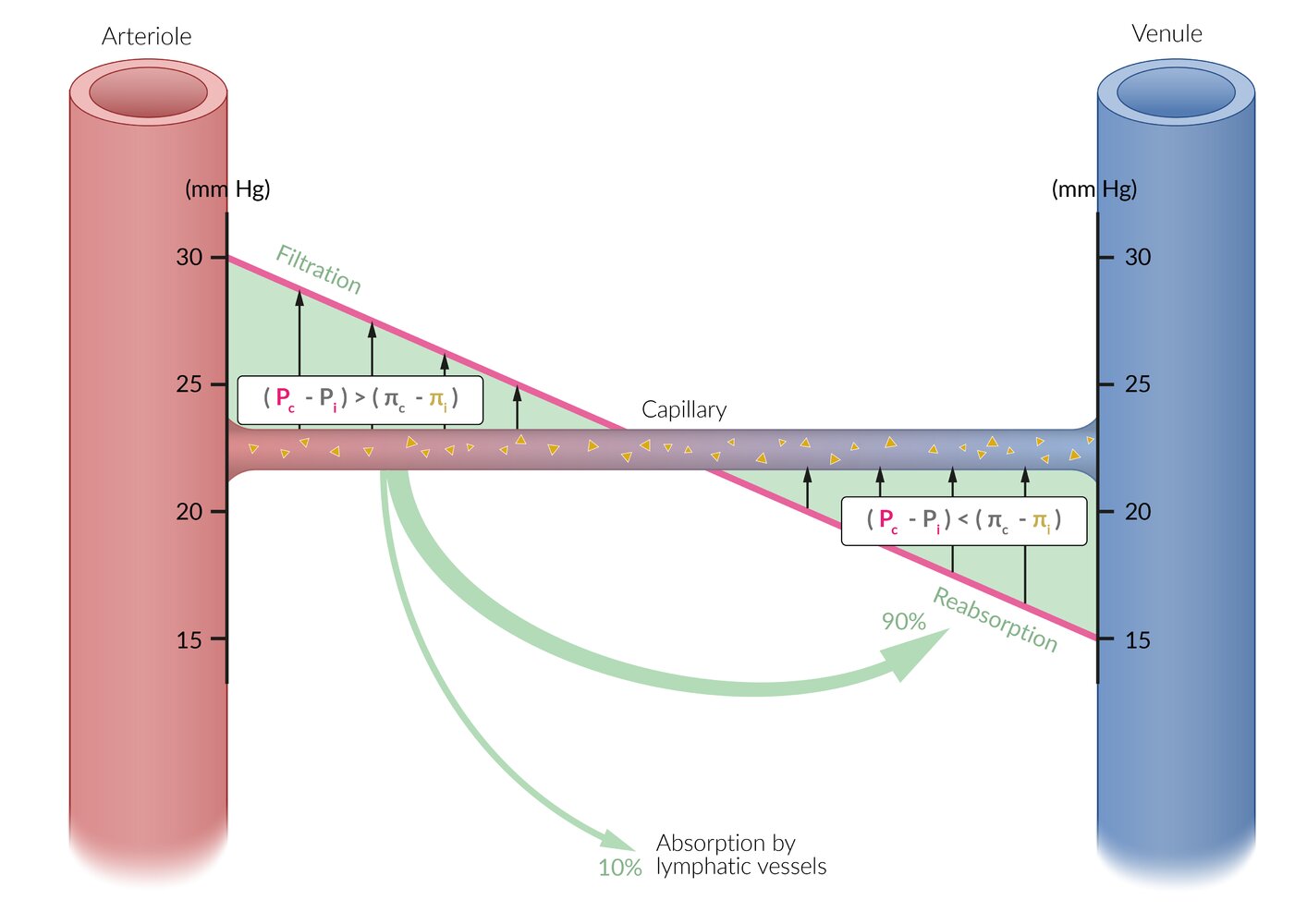
- Edema: abnormal fluid accumulation in the interstitium due to an imbalance in fluid homeostasis caused by either decreased absorption or increased secretion of fluid in the interstitium
-
Peripheral edema: excess fluid in tissues perfused by the peripheral vascular system
- Dependent edema: the accumulation of fluid in the interstitial space in areas of the body influenced by gravity, e.g., the lower limbs in ambulatory individuals and the sacral area in patients who are not ambulatory
- Pitting edema: residual indentation following the application of pressure to the site of the swelling
- Nonpitting edema: no residual indentation following the application of pressure to the site of swelling


Common etiologies by mechanism [1][2]
Some causes of peripheral edema (e.g., pregnancy, cirrhosis) have more than one pathophysiological mechanism. See “Capillary fluid exchange” for more information on vascular physiology.
-
Increased capillary pressure
- Chronic venous insufficiency
- Heart failure
- Medications, e.g., calcium channel blockers
- Pregnancy
- Deep vein thrombosis
- Postthrombotic syndrome
- Cirrhosis
-
Decreased oncotic pressure: resulting from protein deficiency (mainly hypoalbuminemia)
- Protein-losing enteropathy
- Malnutrition
- Nephrotic syndrome
- Cirrhosis
- Pregnancy
-
Increased capillary permeability
- Inflammation
- Infection
- Toxins
- Burns
- Allergic reaction
- Trauma
- Lymphatic obstruction: lymphedema
-
Other: myxedema
- Hypothyroidism (generalized edema)
- Hyperthyroidism (typically pretibial myxedema)
The etiology of peripheral edema is often multifactorial. [3]
Common etiologies by site and acuity
| Etiologies of bilateral vs. unilateral peripheral edema [3][4][5] | ||
|---|---|---|
| Bilateral | Unilateral | |
| Acute (< 72 hours) [3] |
|
|
| Subacute (3 days to 3 months) [3] | ||
| Chronic (> 3 months) [3] |
|
|
Medications that cause edema [2][3]
The following list includes medications that commonly cause edema. It is not exhaustive.
-
Antihypertensives
- Calcium channel blockers, especially dihydropyridines
- Beta blockers
- Clonidine
- Hydralazine
- Methyldopa
- Gabapentinoids
-
Hormones
- Corticosteroids
- Estrogen
- Progesterone
-
Chemotherapy
- Docetaxel
- Gemcitabine
- Pemetrexed
- Lenalidomide, thalidomide
- Anticancer immunotherapy
- NSAIDs
- Thiazolidinediones
- MAO inhibitors
- Pramipexole
Anasarca
- Extreme generalized peripheral edema
- Typically caused by systemic illness, e.g., liver failure, nephrotic syndrome, heart failure, or severe malnutrition
Periorbital edema
- Edema of the soft tissues that surround the orbital cavity
- Usually secondary to trauma, inflammation, protein deficiency (e.g., nephrotic syndrome), or malignancy
Lipedema [6]
- Definition: loose connective tissue disease characterized by the excessive accumulation of nodular and fibrotic fat, primarily in the limbs, hips, and buttocks
- Epidemiology: occurs almost exclusively in women
-
Clinical features
- Symmetrical nonpitting swelling
- Pain, and tenderness in the affected areas
- Spares hands and feet
-
Management includes:
- Weight loss programs: i.e., diet, exercise, and/or bariatric surgery [6]
- Compression garments
- Surgical removal (e.g., liposuction)
Medical history [3][4][5]
-
History of present illness
- Location
- Onset, and tempo
- Exacerbating and alleviating factors
- Associated pain
- Edema from systemic causes: usually painless; sometimes manifests with discomfort and difficulty walking
- Chronic edema: Peripheral polyneuropathy may occur.
-
Evaluation of risk factors
- Risk factors for DVT
- Medications that cause edema
- History of injury, radiation, or surgery to affected limb(s)
Physical examination [3]
-
Peripheral edema
- Location and symmetry of edema
- Examination for pitting edema
-
Skin changes
- Clinical features of chronic venous insufficiency, e.g., stasis dermatitis
- Erythema, warmth
- Myxedema, e.g., scaly nodules and plaques with orange-peel appearance
- Ecchymosis
- Signs of systemic disease, e.g., heart failure, cirrhosis, nephrotic syndrome




Approach [3][4]
Unilateral edema
The approach depends on the duration:
-
≤ 3 months (i.e., acute and subacute peripheral edema):
- Follow the diagnostic approach for suspected lower-extremity DVT.
- Consider evaluation for other etiologies based on clinical suspicion, e.g.:
- Cellulitis
- Trauma, e.g., tibial fracture, ankle fracture, ankle sprain, compartment syndrome
- Ruptured popliteal cyst
- > 3 months (i.e., chronic peripheral edema): Perform diagnostic studies for chronic venous insufficiency.
Unilateral edema does not require a workup for a systemic cause. [5]
Bilateral edema
- Initial evaluation: Evaluate for common causes of peripheral edema based on clinical suspicion.
-
Further evaluation (once systemic causes are ruled out):
- Perform diagnostic studies for chronic venous insufficiency.
- Assess for lymphedema.
- Consider IVC thrombosis in patients with risk factors (e.g., malignancy, thrombophilia).
Laboratory studies [3][4]
Obtain as indicated to evaluate for systemic causes of peripheral edema.
- CMP: liver and/or kidney disease
- TFTs: hyperthyroidism or hypothyroidism
- BNP: heart failure
- Urine protein/creatinine ratio: proteinuria and nephrotic syndrome
Imaging [3][4]
-
Duplex ultrasound (preferred)
- Allows for viewing of venous anatomy, patency, and valve function
- Indications
- Suspected DVT in patients with intermediate or high PTP, or low PTP with positive D-dimer
- Lower extremity edema with negative workup for other causes
- CT or MRI with contrast: if additional imaging is required after duplex ultrasound
-
Venography with intravascular ultrasound
- If previous imaging was inconclusive
- Also used for endovascular treatments
- Lymphoscintigraphy: if lymphedema diagnosis remains uncertain after clinical evaluation
The site of imaging (e.g., lower extremity, pelvis, abdomen) is based on suspected pathology.
| Common causes of peripheral edema [3][5] | |||
|---|---|---|---|
| Condition | Distinguishing clinical features | Diagnostic findings | Management |
| Chronic venous insufficiency (most common cause) |
|
|
|
| Heart failure |
|
|
|
| Lymphedema |
|
|
|
| Nephrotic syndrome |
|
|
|
| Cirrhosis |
|
|
|
| Medication-induced edema |
|
|
|
| Acute DVT |
|
|
|
| Graves disease |
|
|
|
| Hypothyroidism |
|
|
|
| Pulmonary hypertension |
|
|
|
| OSA |
|
|
|
Unilateral edema is usually caused by venous or lymphatic conditions, while bilateral edema is usually caused by systemic conditions. [3]






- Treat the underlying condition.
- Discontinue or reduce dose of causative medications, if possible.
- Encourage lifestyle modifications.
- Exercise
- Elevation of legs when seated
- Weight loss if indicated
- Initiate venous compression therapy. [5]
- Prescribe diuretic therapy to treat systemic fluid overload, e.g., in heart failure, cirrhosis, or nephrotic syndrome. [4]
Diuretics are not indicated for nonsystemic causes of peripheral edema, e.g., lymphedema. [4]
Compression therapy (> 20 mm Hg) is contraindicated in patients with peripheral artery disease with an ankle-brachial index < 0.7. Always measure an ankle-brachial index before starting compression therapy. [4][5]