Tubulointerstitial diseases are conditions of inflammation of the renal tubules and interstitium that can lead to renal failure. Acute tubulointerstitial nephritis (ATIN) is the third most common cause of acute kidney injury (AKI) in hospitalized patients after acute tubular necrosis (ATN) and prerenal AKI, and it is most commonly caused by an allergic reaction to medications. ATIN commonly manifests with a slowly progressive, nonoliguric, intrinsic AKI. The classic triad of fever, morbilliform rash, and eosinophilia is seen in < 10% of cases. Laboratory study findings may suggest interstitial nephritis, but histological confirmation with renal biopsy is required for a definitive diagnosis. Early recognition, removal, or treatment of the suspected cause, and, in select cases, administration of glucocorticoid therapy, will result in complete or partial resolution for most patients, while a minority of patients experience irreversible kidney damage. Chronic tubulointerstitial nephritis (CTIN) is commonly due to the progression of ATIN, but it may also be caused by medications, infections, toxins, or systemic diseases. Treatment involves managing or eliminating the underlying cause and management of CKD. Crystal-induced nephropathy is a type of kidney damage that results from crystal deposition in the renal vasculature, the renal tubules, or the draining urinary tract and that may lead to crystal-induced AKI, crystal-induced CKD, or urolithiasis. Renal papillary necrosis, a necrosis of the renal medullary pyramids and papillae, is caused by ischemia (due to, e.g., sickle cell disease and sickle cell trait, acute pyelonephritis, or obstruction of the urinary tract). Patients often present with AKI with hematuria and sloughed papillae. Management should include treatment of the underlying cause, IV fluids to prevent blood clot formation and upper urinary tract obstruction, and management of further complications.
Definition
Acute tubulointerstitial nephritis (ATIN) is an acute inflammation of the renal interstitium and tubules that causes a decline in renal function over a period of days to weeks. [1]
Epidemiology
- Third most common cause of AKI in hospitalized patients [2]
- Seen in ∼ 15% of biopsy samples obtained for unexplained AKI [3]
Pathophysiology
- Immune-mediated tubulointerstitial damage (allergic interstitial nephritis) is the most widely accepted theory.
- Inflammatory infiltrates → tissue edema and tubular cell damage → compromised tubular flow
- Allergic interstitial nephritis: drugs act as haptens → type IV hypersensitivity reaction [4]
- Acute obstruction: crystals (from e.g., uric acid, medications) or proteins (e.g., light chains) obstruct tubules
Etiology [1][5][6]
-
Medications (most common) [2]
- Antibiotics: β-lactams, sulfonamides, rifampin, fluoroquinolones
- NSAIDs
- Proton pump inhibitors and H2 blockers
- Loop diuretics and thiazides
- Anticonvulsants: phenytoin, valproate, carbamazepine, phenobarbital
- Other: allopurinol, immune checkpoint inhibitors (e.g., nivolumab, pembrolizumab), mesalamine
-
Infection
- Bacteria
- Escherichia coli, Brucella spp., Campylobacter spp., Salmonella spp., Streptococcus spp., Staphylococcus spp., Legionella spp.
- Spirochetes (e.g., Leptospira, Treponema pallidum)
- Mycobacteria, mycoplasma
- Viruses: HIV, CMV, EBV, HSV, measles, mumps, hantavirus
- Other
- Parasites (e.g., Toxoplasma, Leishmania)
- Fungi (e.g., Histoplasma, Coccidioides)
- Bacteria
- Autoimmune: Sjogren syndrome, sarcoidosis, SLE, tubulointerstitial nephritis with uveitis, IgG4-related systemic disease [7]
- Other: autosomal dominant tubulointerstitial kidney disease
“Please RSVP:” Rifampin, Sulfa drugs and the V (5) Ps (Proton pump inhibitors, Pain killers (NSAIDs), “Pee pills” (diuretics), Penicillins, and Phenytoin) are the drugs that cause acute tubulointerstitial nephritis.
Clinical features [2]
-
Clinical features of acute kidney injury, with or without:
- Morbilliformrash
- Fever
- Arthralgias
- Flank pain
The classic triad of fever, morbilliformrash, and eosinophilia is present in < 10% of patients with ATIN, but their presence can help to guide the diagnosis. [2][6]
Diagnostics [8][9]
Approach
- Determine if the patient fulfills diagnostic criteria for AKI.
- Obtain a minimum diagnostic workup for patients with suspected kidney diseases.
- Blood tests and urine studies
- Renal imaging studies
- Identify characteristic clinical features, risk factors, and potential exposures for ATIN.
- Consider renal biopsy (gold standard test) if there is no improvement under supportive care.
ATIN typically manifests as slowly progressive, nonoliguric, intrinsic AKI. However, patients with severe disease may present with oliguria and the course may be rapidly progressive. [4]
Blood tests [2][3][6]
- BMP: : ↑ BUN and creatinine
- CBC: : ↑ eosinophils (more common in drug-induced ATIN)
Urine studies [2][3][6]
-
Urinalysis
- Sterile pyuria
- Subnephrotic-range proteinuria
- Microscopic hematuria
-
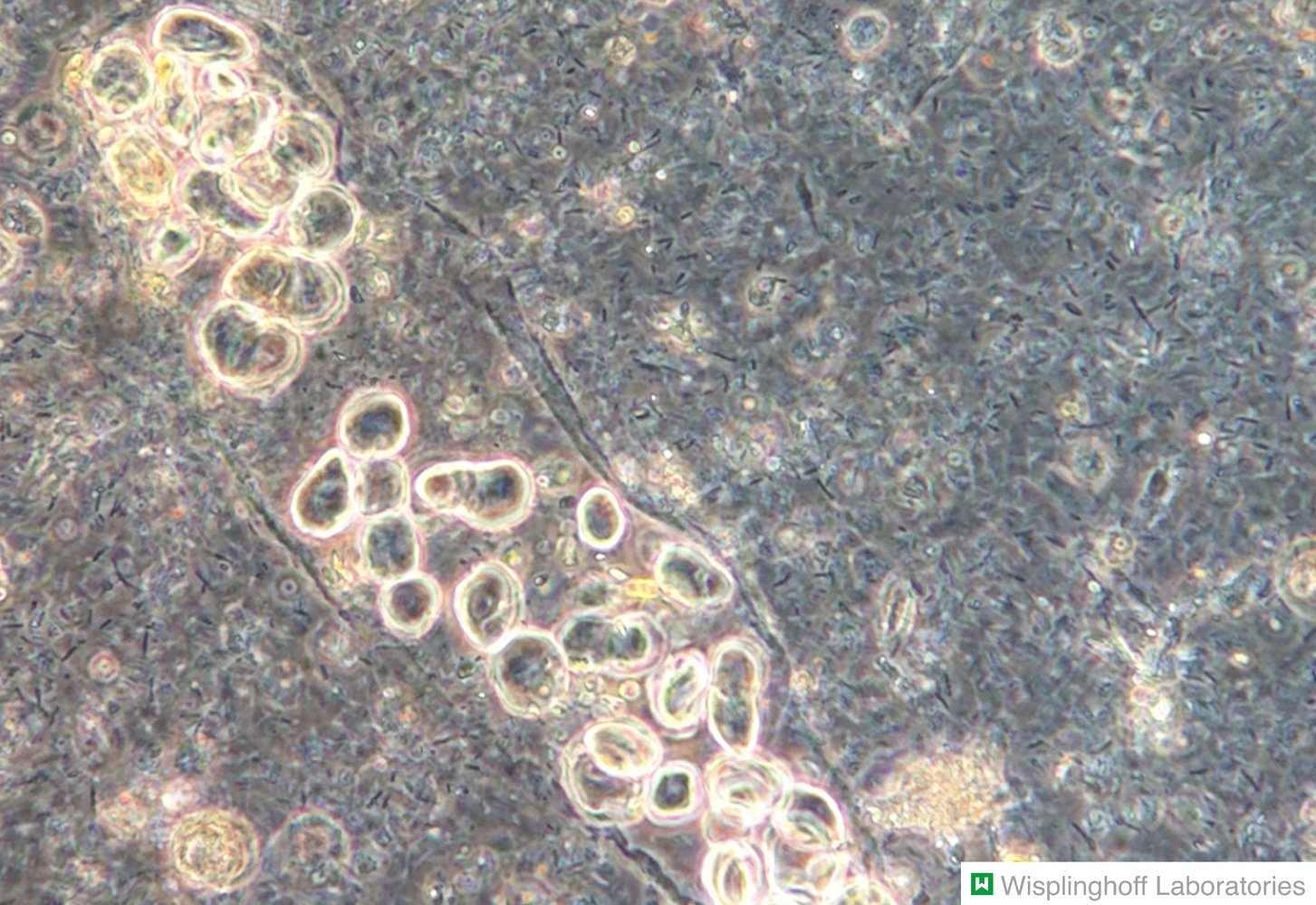
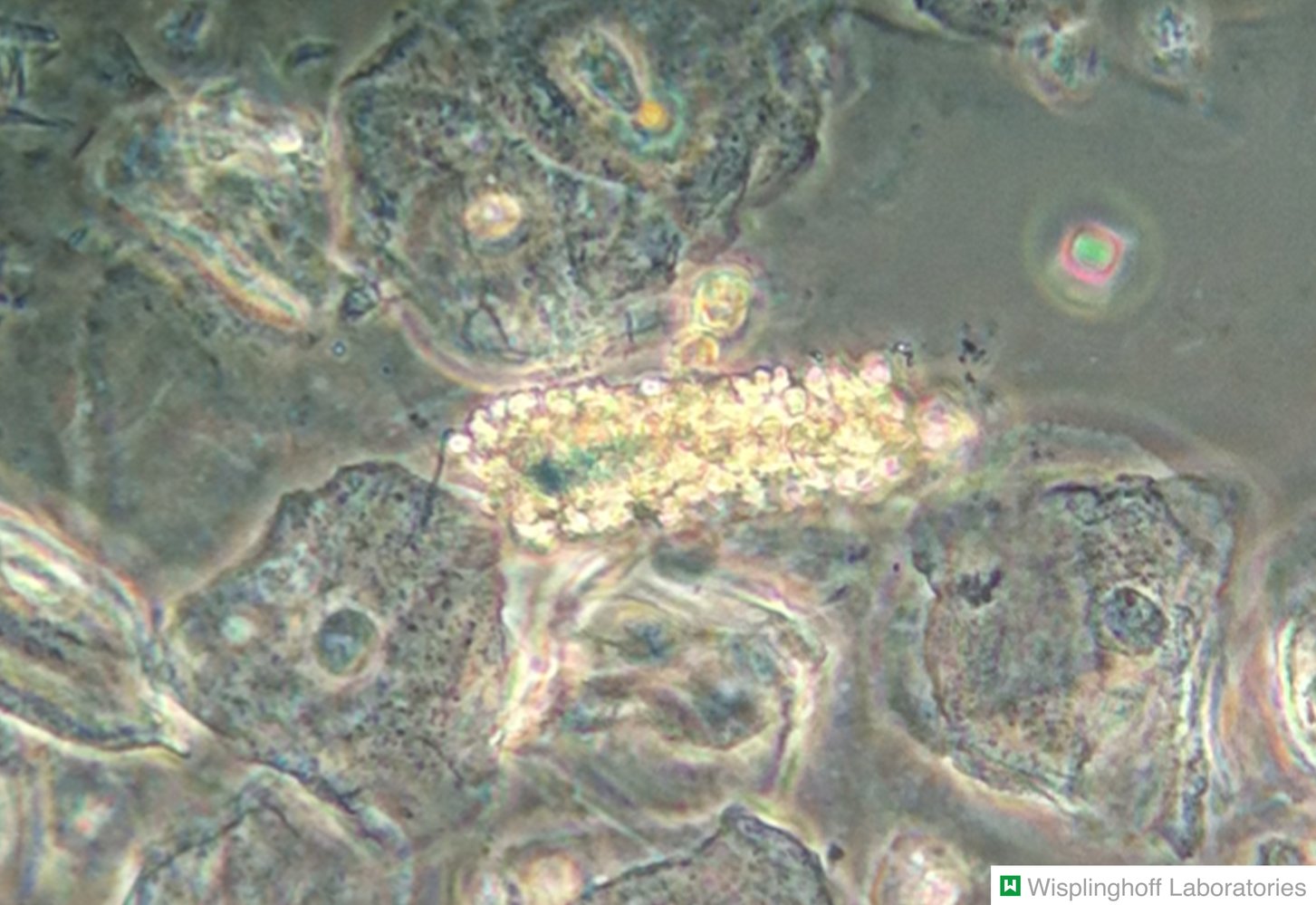
Urine microscopy
- Up to 20% of patients have bland urine sediment.
- WBC casts, RBC casts, waxy casts, granular casts, tubular epithelial casts
- Urine eosinophils (low sensitivity and specificity for ATIN) [10]
-
Urine chemistries in tubulointerstitial disease (findings depend on the major site of injury) [3][11]
- Medullary defects: e.g., urine concentrating defects (nephrogenic diabetes insipidus), sodium wasting
- Proximal tubular defects: e.g., glycosuria, phosphaturia, bicarbonaturia, natriuresis, findings of type 2 renal tubular acidosis
- Distal tubular defects: e.g., natriuresis, hyperkalemia, findings of type 1 renal tubular acidosis
Although frequently cited as a diagnostic clue, in clinical practice, urine eosinophils lack sensitivity and specificity for reliably confirming ATIN. [12]



Renal ultrasound [5]
- Indication: to rule out other causes of AKI
-
Findings
- Often normal
- May demonstrate enlarged kidneys with increased echogenicity, reflecting interstitial edema [3]

Renal biopsy [6][13]
-
Indications include:
- No improvement or the patient worsens after 3–5 days of supportive care and withdrawal of potential causative agent.
- Guiding treatment of suspected causes
-
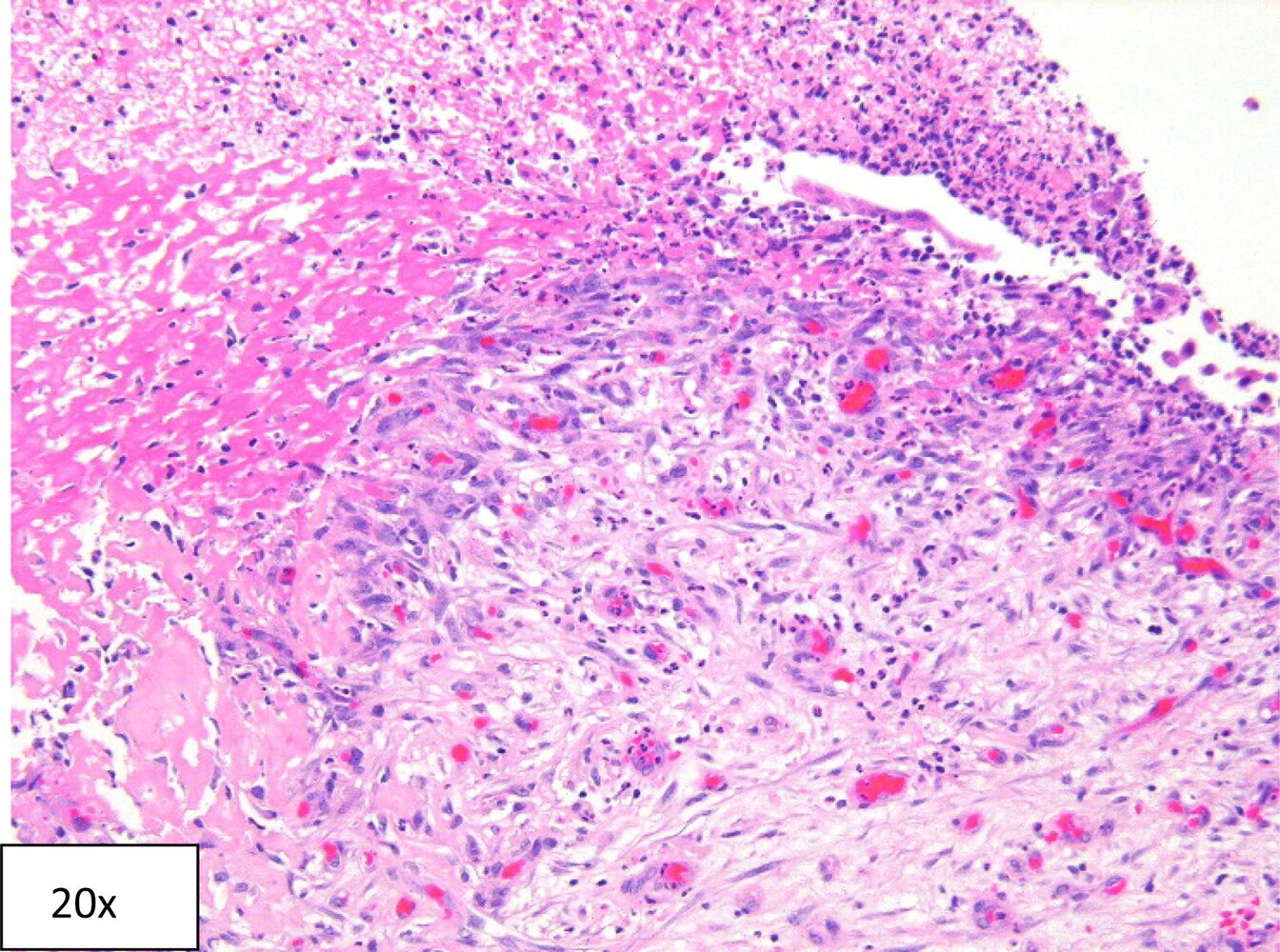
Findings
- Diffuse or patchy peritubular inflammatory cell infiltrates: T-cell lymphocytes and monocytes (macrophages, eosinophils, and plasma cells)
- Interstitial edema
- Sparing of glomeruli and vessels
Differential diagnoses [5]
- Other causes of intrinsic AKI
- Crystalline nephropathy
- Acute tubular necrosis
- Vasculitis
- Atheroembolic disease
- Glomerulonephritis
- DRESS syndrome
- Prerenal AKI
- Postrenal AKI
ATIN, atheroembolic disease, vasculitis, and DRESS syndrome can all manifest with AKI, skin lesions (e.g., livedo reticularis, purpura, or rash), and eosinophilia, and should be considered as differential diagnoses. [6]
Management [1][8][13]
- Stop causative agents or treat underlying systemic disease.
- Provide supportive care for AKI; for 3–5 days.
- Consider systemic glucocorticoids under specialist guidance.
- Monitor kidney function; evaluate for indications for acute dialysis.
Glucocorticoid therapy [6][14]
-
Common indications
- Specific ATIN etiologies, e.g.:
- Drug-induced AIN
- Autoimmune disorders
- Postinfectious ATIN with delayed recovery
- Insufficient improvement in eGFR after 3–5 days of supportive care for AKI
- Impending indication for dialysis
- Diffuse infiltrates and no extensive fibrosis on biopsy sample
- Specific ATIN etiologies, e.g.:
- Example regimen (off-label) : methylprednisolone followed by prednisone [14]
-
Important considerations
- There is a paucity of high-quality evidence to support the use of glucocorticoids in ATIN.
- When indicated, glucocorticoids should be started within 7 days of diagnosis. [6][14]
- Consider stopping glucocorticoids if there is no improvement in renal function after 1 week of therapy.
Definition
Chronic tubulointerstitial nephritis (CTIN) is a condition of chronic inflammation of the renal tubules and interstitium and can progress to end-stage renal disease (ESRD) after months or years. [15]
Pathophysiology [11]
- Interstitial mononuclear cell infiltration → tubulointerstitial fibrosis and atrophy → glomerular and vascular fibrosis and sclerosis → chronic kidney damage
- Pathophysiology of specific causes of CTIN includes:
- Progression of ATIN: chronic inflammation → fibrosis → chronic renal damage
-
Analgesic nephropathy (e.g., resulting from NSAID use)
- Inhibition of prostacyclinsynthesis →vasoconstriction of the medullary blood vessels →papillaryischemia and papillary necrosis [16]
- Associated with an increased risk of urothelial carcinoma; can progress to ESRD [16]
- Reflux nephropathy: chronic high-pressure reflux and recurrent UTIs → tubular atrophy and patchy interstitial fibrosis [5]
- Myeloma cast nephropathy: Excessive amounts of light chains are produced and filtered into the primary urine →precipitation of light chains in renal tubules → tubular obstruction
Epidemiology [11]
- The overall prevalence of CTIN is unknown.
-
Chronic interstitial nephritis in agricultural communities (CINAC) : [17]
- CTIN with secondary glomerulosclerosis; primarily seen in young male agricultural workers
- Prevalence approaches epidemic proportions (15%) in Sri Lanka, some countries in Central America, and other countries with a tropical climate.
Etiology [5]
-
Medications
- Analgesic nephropathy; : combination analgesics, NSAIDs, and acetaminophen
- Calcineurin inhibitors: cyclosporine, tacrolimus
- Chemotherapeutic agents: cisplatin, ifosfamide
- Nucleoside inhibitors: cidofovir, tenofovir
- Aristolochic acid: causative agent in aristolochic acid nephropathy
- Other: mesalamine, lithium
- Toxins: lead; (i.e., chronic lead nephropathy), cadmium
- Infections: chronic pyelonephritis, tuberculosis
- Systemic diseases: multiple myeloma, Sjogren syndrome, SLE, sickle cell disease, vasculitis, sarcoidosis, lymphoma, IgG4-related systemic disease, tubulointerstitial nephritis with uveitis
- Metabolic diseases: hyperuricemia, hypercalcemia, hyperoxaluria, hypokalemia
-
Miscellaneous
- Radiation nephritis
- Kidney graft rejection
- Hypertension
- Ischemia
- CINAC
Clinical features [5][9]
CTIN typically follows an indolent course. Clinical features vary according to the etiology.
- Painless hematuria, pyuria, oliguria, or polyuria
- Colicky flank pain
- Uremia or other symptoms of chronic kidney disease
- Symptoms of an underlying condition (e.g., symptoms of multiple myeloma)
- Type II RTA with Fanconi syndrome resulting from defects in proximal tubules
- Type IV RTA resulting from defects in distal tubules
Analgesic nephropathy increases the risk of urothelial carcinoma and can progress to ESRD. [16]
Diagnostics [5][9][18]
Perform a diagnostic workup for CKD and evaluate for risk factors and exposures that suggest CTIN (see “Etiology”).
-
Laboratory studies
- Obtain BMP, CBC, urinalysis, urine microscopy, and urine chemistries for all patients.
- Findings
- Blood tests: ↑ BUN and creatinine, ↓ K+ or ↑ K+; normal anion gap; anemia of CKD [2][3]
- Urine chemistries in tubulointerstitial diseases (findings similar to ATIN): sterile pyuria, proteinuria, hematuria; , RBC casts, WBC casts [2][3][6]
-
Renal ultrasound [9]
- Obtain to rule out other causes of CKD (not used to confirm or exclude the diagnosis of CTIN).
- Findings
- Typically, small kidneys with increased echogenicity
- Normal to large echogenic kidneys may be seen in infiltrative tubulointerstitial diseases (e.g., sarcoidosis, lymphoma).
-
Renal biopsy [6][9]
- Can be used to diagnose specific causes that would alter management or help determine the prognosis
- Findings include tubulointerstitial fibrosis and tubular atrophy.
Laboratory findings in chronic tubulointerstitial nephritis have significant overlap with other causes of CKD and are neither sensitive nor specific.
Differential diagnoses
See “Etiology of chronic kidney disease.”
Treatment [18]
Treatment consists of management of CKD, including treatment of the underlying cause.
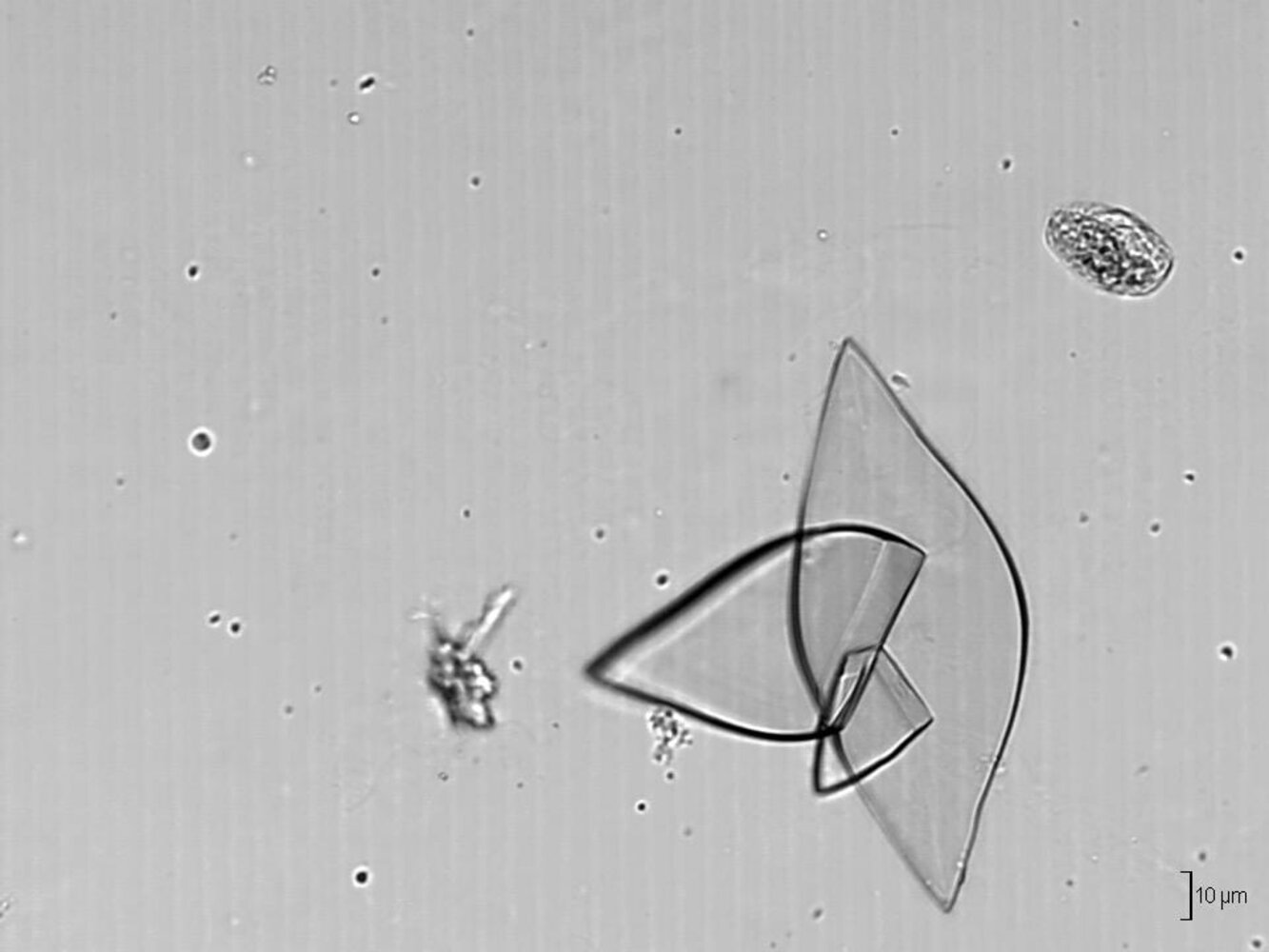
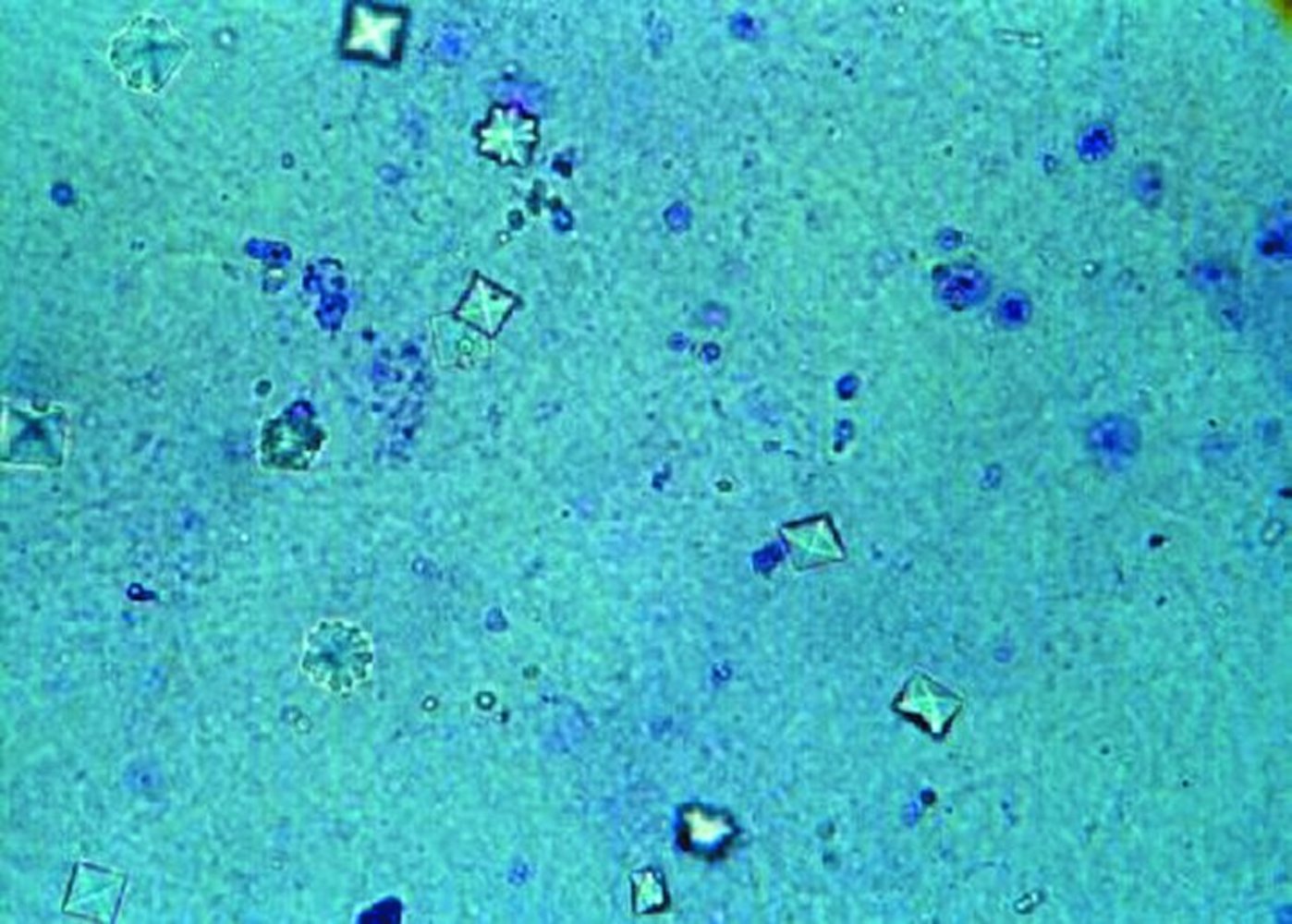
- Definition: : a type of kidney injury that is triggered by crystal deposition and may lead to crystal-induced AKI, crystal-induced CKD, or urolithiasis
-
Pathophysiology
- Precipitation of minerals (crystallization) → phagocytosis of crystals → activation of the inflammasome → renal damage
- Precipitation of minerals (crystallization) → obstruction of tubules → renal damage
| Overview of crystalline nephropathies [19][20] | |||
|---|---|---|---|
| Renovascular crystallopathy | Tubular crystallopathy | Urolithiasis | |
| Pathophysiology |
|
|
|
| Etiology |
|
|
|
|
|
||
| Clinical features |
|
|
|
| Diagnostics |
|
||
| Management |
|
||
Definition
Renal papillary necrosis is ischemic, coagulative necrosis of the renal medullary pyramids and papillae and is a feature of various conditions.
Pathophysiology
- Ischemia →necrosis and sloughing of the papillae → ureteral obstruction → possible scarring
- Usually bilateral; can also affect a single papilla [21]
Etiology
- Often multifactorial
- Sickle cell disease and sickle cell trait
- Acute pyelonephritis
- Obstruction of the urinary tract
- Tuberculosis
- Cirrhosis of the liver
- NSAIDs (due to inhibition of prostaglandin-mediatedvasodilation in the vasa recta)
- Renal transplant rejection
- Diabetes mellitus
- Systemic vasculitis
POSTCARDS: Pyelonephritis, Obstruction, Sickle cell disease, Tuberculosis, Cirrhosis, Analgesics (NSAIDs), Renal transplant rejection, Diabetes mellitus, and Systemic vasculitis are the causes of renal papillary necrosis.
Clinical features
-
Acute
- Flank pain, colicky pain
- Hematuria (microscopic or macroscopic)
- Proteinuria
- Fever, chills
- Acute kidney injury
- Chronic: : usually asymptomatic or mild symptoms
Diagnostics [11][22]
Consider renal papillary necrosis as part of the differential diagnosis for patients presenting with hematuria, particularly if risk factors are present (e.g., sickle cell disease, diabetes, chronic oral analgesic use).
Laboratory studies
- BMP: ↑ BUN and creatinine
-
Urine studies [23][24]
- Gross or microscopic hematuria
- Proteinuria
- Sterile pyuria
- Sloughed papillae
Imaging studies [21][22]
Obtain in all patients to assess for ischemic changes and exclude differential diagnoses or precipitating conditions (e.g., kidney tumors, pyelonephritis, nephrolithiasis).
-
CT urography [21][22][25]
-
Test of choice for renal papillary necrosis
- Can visualize early ischemic changes (while they may still be reversible)
- Useful for differential diagnosis
- Findings (during the contrast excretory phase) [26]
- Small, contrast-enhancing papillary cavities abutting the calices
- Filling defects in the renal pelvis due to irregular (e.g., necrotic or peripherally calcified) papillae
- Small kidneys in chronic nephritis
-
Test of choice for renal papillary necrosis
-
Renal ultrasound [21]
- Quick, noninvasive initial test to assess for hydronephrosis, tumors, or calculi
- Findings: increased echogenicity of the inner medulla; filling defect in the medullary tip (late finding)
-
Intravenous urography [22]
- Historically considered the test of choice; CT urography is now preferred.
- Findings: may be normal initially; see findings of CT urography above.
Treatment [11]
- Treat the underlying cause: See “Etiology.”
- Prevent blood clot formation: Provide IV fluid therapy to maintain high urine output.
-
Manage complications if present.
- Management of AKI: e.g., supportive care for AKI; consider indications for acute dialysis.
- Treatment of pyelonephritis: e.g., antibiotic therapy
- Treatment of upper urinary tract obstruction: e.g., ureteral stenting
- Management of massive hemorrhage (rare), e.g.:
- Type and screen and pRBC transfusion as indicated
- In refractory or severe cases: radiographic or percutaneous embolization, or surgical nephrectomy